Elevator pitch
Large and sudden economic and political changes, even if potentially positive, often entail enormous social and health costs. Such transitory costs are generally underestimated or neglected by incumbent governments. The mortality crisis experienced by the former communist countries of Europe—which caused ten million excess deaths from 1990 to 2000—is a good example of how the transition from a low to a high socio-economic level can generate huge social costs if it is not actively, effectively, and equitably managed from a public policy perspective.
Key findings
Pros
Acute psychosocial stress was one of the main drivers of the sharp mortality increase experienced by the former communist countries of Europe.
In central Europe, the post-communist mortality crisis was quickly solved, while in much of the former USSR, life expectancy at birth did not return to 1989 levels until 2013.
The relative success of central European countries in recovering from health shocks after the transition from communism indicates how this type of mortality crisis can be avoided in the future.
Cons
In most countries, analyses of the mortality impact of the transition have only had a modest impact on public policy.
The formulation of a single causal model to explain the causes of the post-communist mortality crisis is difficult because key explanatory variables belong to different disciplines.
Data on alcohol and stress during the transition away from communism are patchy at best—a fact that inhibits conclusive testing about their relative impact on mortality.
The transition mortality crisis primarily affected marginal groups such as the unemployed, single, young, and middle-aged men and women with limited education and skills, who lived in or migrated to urban areas under stressful conditions.
Author's main message
The transition of Europe’s communist countries to market-based economies was universally greeted as a key step toward world peace and economic progress. However, unlike the experiences from China and Vietnam, the European transition was characterized by a severe transformational recession and an acute mortality crisis. This mortality crisis was due to acute stress experienced by the weakest sections of the population during a period of exceptional instability. To mitigate future potential crises, policymakers should focus on job re-training, public works, unemployment compensation, wage subsidies, and policies that could prevent spikes in inequality, social exclusion, family breakups, and distress migration.
Motivation
The beginning of 1989 marked the onset of the epochal transformation of Europe’s former communist countries into liberal democracies. While the months preceding this historic watershed moment were characterized by great expectations, the subsequent years brought about an unprecedented fall in output, mass impoverishment, and rising inequality.
The mortality impact of these developments was dramatic. During the first reform years, male—and to a lesser extent female—life expectancy at birth (LEB) fell in all of Europe’s former communist countries. It rebounded in central Europe from 1991 to 1993 and in the Baltic States from 1995 to 1996. However, in Russia, Ukraine, and Belarus, health status remained precarious until the mid-2000s. Since then, male LEB has recorded widespread gains also in these three countries; but, only in 2013 did their LEB reach its 1989 levels, and it was only just above those levels in another five former communist countries. Despite its magnitude, the post-communist European transition mortality crisis has attracted little attention from national authorities or international agencies.
Discussion of pros and cons
The relevant literature includes studies that attempt to clearly document and explain the post-communist European mortality crisis, which was one of the worst peacetime demographic crises of the 20th century. Teams of demographers, economists, epidemiologists, and policy analysts worked together to conduct the most useful analyses, as only multidisciplinary teams are capable of explaining such a complex phenomenon [2]. Over the past decades several theories have been proposed for why this crisis occurred, and there is now broad consensus that its main triggering factors were acute stress and an increased consumption of stress relievers—first and foremost, alcohol.
Yet, despite general agreement on the main contributing factors, the formulation of a unified causal model to explain the European transition mortality crisis has remained difficult, primarily due to the fact that the variables used to analyze its causes belong to disciplines that adopt different research methodologies and approaches. In addition, data for several key variables (e.g. unemployment and family disruption) are only available at the aggregate level, while for others (e.g. stress and alcohol consumption), data coverage is patchy at best—a fact that prohibits a precise understanding of their relative impact on health.
One of the more surprising findings of the transition mortality crisis is the difference in the gravity of the crisis experienced by central Europe versus that of the countries of the Former Soviet Union (FSU). In the latter countries, analyses of the transition health crisis generated a very limited policy response by incumbent governments, a fact that raises questions about the degree of democratization and social concern prevailing in these nations.
Features of the transition mortality crises
During 1989−1991, male LEB fell in 16 of the 21 former communist countries included in Figure 1 and Figure 2. Even in central Europe, loss of human life was sizable from a welfare perspective, though not in long-term demographic trends. For instance, in 1990−1991 Poland recorded 8,400 excess male deaths, while Hungary registered 10,300 excess male deaths and 3,400 excess female deaths over 1990−1993 [2]. After this initial surge, mortality rates declined (see Figure 1) due to less marked and shorter recessions, smaller inequality rises, the introduction of active labor market programs, an increase in public expenditure on health, stagnation of alcohol consumption, and limited changes in family stability.
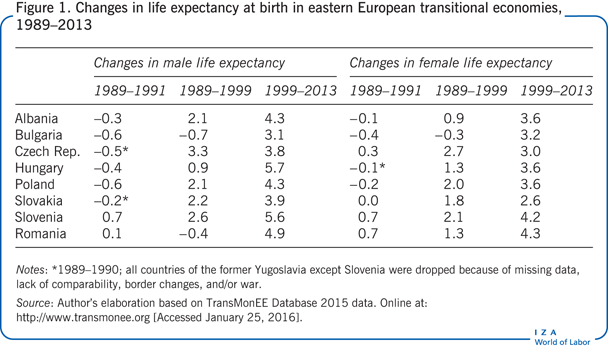
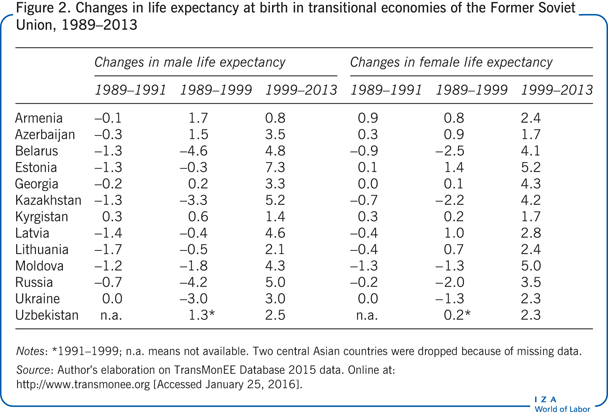
The mortality crisis was much more acute in south-east Europe (Albania, Bulgaria, and Romania) (see Figure 1) and the FSU than in central Europe (see Figure 2). As a result, by 1994, the LEB of Russian males had fallen to 57.6 years, 6.6 years less than it was in 1989, and even 3 years less than that of India, which was at that time a poor agrarian country. By 1999, male and female LEB was still lower than the 1989 levels in 10 and 6 of these countries, respectively (see Figure 2). Of particular concern was the situation in Belarus, where both male and female LEB had declined for ten consecutive years by 1999.
With a return to stability, growth, and employment creation from 1999 to 2013, the central European, Baltic, and a few central Asian countries registered male and female LEB improvements of 0.2−0.4 years per annum. In contrast, the gains recorded in Russia, Ukraine, Belarus, Armenia, Lithuania, and Kazakhstan were close to zero. As a result, in 2013, male LEB had barely returned to its 1989 levels in Russia, Ukraine, and Belarus, and had exceeded them by only 1.6−2.5 years in another six FSU and south-east European countries. A new mortality gap has thus emerged between Russia and its former satellites (see Figures 1 and 2). It is important to understand why, in an era of growing opportunities associated with the market economy, many FSU countries remain far behind those of central Europe. On a positive note, the rapid reduction in cardiovascular mortality in Russia that began in 2004 has started to close this health gap.
Population groups affected and immediate causes of death
Looking back, it could have been expected that the European mortality crisis would primarily have affected children, pregnant women, the elderly, and the disabled. Yet, as shown in Figure 1 and Figure 2, men were much more affected than women in every transition country. The fastest relative upswing in mortality was recorded for 20−39 year olds, who experienced a marked rise in violent deaths, while the fastest absolute rise occurred among 40−59 year olds, who were mainly affected by a rise in cardiovascular deaths [3]. In contrast, people over 60 did not experience any rise in mortality. As for the level of education, past studies have documented the steep mortality gap between people with different levels of education. Higher education allows one to process new information more easily, facilitates employment mobility, and enables better use of limited resources. Education also increases awareness about the risks associated with unhealthy behaviors. Evidence from the early 1990s confirms these findings, as it shows that mortality differentials by level of education widened during the transition. For instance, the temporary life expectancy gap in Russia between the best and least educated males aged 20−69 rose from 1.63 to 1.89 between 1988−1989 and 1993−1994 [3].
Stress-related mortality is highest among people who live alone. From 1992 to 1994, a surge in the number of widows and widowers, a drop in marriage rates and—in the Slavic countries of the FSU—an increase in divorce rates, raised the number of adults living alone. Death rates also rose due to an increased prevalence of distress migration following the breakdown of states, the return of troops posted abroad, and an inflow of refugees fleeing ethnic strife.
Finally, mortality grew faster among the unemployed. Controlled studies have shown that sudden job loss is a cause of stress, cardiovascular and mental problems, and death. Grouped data for the transition economies confirms the existence of a correlation between rises in unemployment and job turnover and mortality increases in the Czech Republic, Russia, Latvia, the former German Democratic Republic, and Poland [3]. Summing up, the evidence suggests that the mortality crisis mainly affected weaker social groups including people who were unemployed, lived alone, belonged to the young or middle-age population cohorts, had limited education and skills, and lived in or migrated to urban areas under stressful conditions.
It is additionally interesting to understand which illnesses and behaviors most impacted the decline in LEB in post-communist Europe. Forty percent of the decline in male LEB, and a non-negligible share of the fall in female LEB, were due to ischemic heart diseases, circulatory problems, and strokes. Beyond illnesses, external causes of death (e.g. poisoning, accidents, suicide, and homicide) explain a large part of the increase in mortality among young men, especially in the FSU. The transition was indeed characterized by a surge in deaths due to motor, train and plane accidents, alcohol and other types of poisoning, drowning, fires, and accidents at work. These types of deaths are those that were directly affected by the collapse of communist state institutions and the erosion of safety standards at work. A third, more limited, increase in mortality was due to an upsurge in deaths related to ulcers and liver cirrhosis. In turn, the “diseases of poverty” (i.e. infectious, nutrition-related, parasitic, and sexually transmitted) rose among vagrants, drug users, and commercial sex workers who were typically not reached by public health systems. Yet, as this rise took place from a very low level, it explains little of the aggregate mortality rise. Finally, respiratory deaths followed a declining trend while cancer deaths showed a slow trended rise.
Causes of the post-communist European mortality crisis
Explanations of limited relevance
In Russia and Ukraine, the rise in mortality during the 1990s has typically been attributed to “cohort effects,” that is, the delayed consequences of debilitation experienced by people born during the 1929−1934 famine or World War II. However, analyses of cohort mortality in Ukraine and Russia suggest that while such cohorts did experience higher mortality rates than adjacent cohorts, this increase explains only a tiny fraction of the total surge in deaths experienced in the 1990s [3]. Even more telling, the proportional increase in death rates was much higher for 20−40 year olds, that is, cohorts born during a period of relative prosperity, and for areas that were unaffected by the demographic shocks of the first part of the 20th century.
A similar explanation was offered by the “postponed death hypothesis,” which suggests that the liberalization of alcohol sales in 1989 led to a large increase in consumption that proved lethal for socially weak people, whose lives had essentially been saved by Gorbachev’s anti-alcohol campaign (which ended after the political transition) [4]. Also, in this case, a comparison of LEB gains during the anti-alcohol campaign and its subsequent rise from 1989 to 1994 suggests that this hypothesis explains only part of the surge in deaths during that period [3]. Moreover, such a hypothesis cannot explain the 2.6-year decline in male LEB that took place from 1998 to 2002 in the aftermath of the Ruble crisis and Russian debt default.
Another hypothesis emphasized the effects of “recession-induced malnutrition.” Prior to the transition, average food intake was very high, meaning it could be reduced without causing nutritional damage. In addition, there was ample opportunity to substitute expensive nutrients with cheaper ones. Considering this, even large reductions in food consumption expenditure cannot have caused a rise in deaths due to under nutrition, except perhaps for a small group of vagrants for whom a surge in poverty-related deaths was basically due to reduced access to shelter, basic hygiene, and health care [3]. Most transition economies also suffered a worsening of the health care system, as public health spending contracted by 15−30% in Russia, Ukraine, Latvia, and Lithuania. In these countries, a rise in deaths among hospitalized patients indicates that such spending cuts played some role in raising mortality. Yet, these cannot explain why mortality increased faster among men, and why it surged mainly for non-amenable causes.
Another explanation focused on the “worsening of lifestyles” (i.e. diet, smoking, and drinking). Yet, according to this viewpoint, mortality should have risen slowly (and not sharply, as it did) as a result of protracted exposure to risky behaviors. Moreover, changes in relative prices and improvements in trading increased consumption of minerals and vitamins while consumption of meat and diary products fell along with the intake of unhealthy saturated fats. Furthermore, from 1989 to 1995, tobacco consumption stabilized (rather than increased), as incomes dropped, the price of imported cigarettes soared, and long-term educational campaigns started generating an impact.
More plausible explanations
More recent analyses have focused on alcohol consumption and acute psychosocial stress as the main drivers of the mortality crisis [3], [5]. However, these studies all highlight that a significant share of the mortality increase remains unexplained.
Mounting alcohol consumption. In view of the unreliability of official sales statistics, alcohol intake is estimated indirectly based on the increase in alcohol-related deaths. This method suggests that alcohol consumption per capita rose in Russia from 11.8 to 14.5 liters per annum between 1989 and 1993, and that it rose in Poland from 8 to 11 liters from 1988 to 1991. These estimates conclude that in Russia, Lithuania, and Poland 32%, 40%, and 27%, respectively, of the surge in male mortality from 1989 to 1994 can be tentatively attributed to increased alcohol intake [3].
Subsequent analyses have focused on the way alcohol is consumed. For example, significant amounts of alcohol are consumed every day in Mediterranean countries, mainly with meals; while in Russia, Belarus, Ukraine, and the Baltics, the same weekly amount is likely to be consumed on a single occasion, a drinking pattern termed “binge drinking.” Research suggests that the latter is causally associated with cardiovascular death. However, a study of 25,000 autopsies carried out in Barnaul (Siberia) from 1990 to 2004 suggests that 21% of adult male deaths that had been attributed to circulatory diseases were actually caused by alcohol poisoning, that is, lethal or near-lethal levels of ethanol concentration in the blood [6]. Thus, for this group of people the cause of death was neither cardiovascular problems nor increased alcohol consumption per se, but rather the uncontrolled manufacturing and sale of dangerous alcohol products.
The key question in this debate is why alcohol consumption increased and became so much more lethal. Possible explanations include: a long-term rising trend (briefly interrupted during the Gorbachev era) reflecting deeply rooted consumption habits; changes in incomes and relative prices of alcohol; a relaxation of anti-alcohol policies; and, acute psychosocial stress that people tried to control by drinking. According to this view, alcohol intake can be seen as an important intermediate cause of the FSU’s mortality crisis. However, the “alcohol hypothesis” does not fully explain why alcohol-related mortality fell during the successful transition experienced by the Czech Republic. Similarly, alcohol-related deaths fell in Russia and the Baltics during the 2000s, even though there was no evidence of a drop in alcohol intake; a drop in the consumption of hard liquors and a subsequent rise in that of beer and wine might explain this observation. Finally, the alcohol hypothesis cannot fully explain the huge rise—and subsequent fall—in cardiovascular and other deaths, which, while related to stress, are only partially mediated by alcohol intake.
Acute psychosocial stress. Acute psychosocial stress is increasingly recognized as a key factor in deaths due to heart problems and hypertension, alcohol psychosis and neurosis, homicide, suicide, accidents, and cirrhosis. These are all causes of death that increased in relative importance during the transition. According to Serafino (1994) cited in [7]: “Stress is the condition that results when person/environment transactions lead the individual to perceive a discrepancy—whether real or not—between the demands of the situation and resources of the person’s biological, psychological or social systems.”
Epidemiological research has shown that—in the absence of mitigating measures—acute stress leads to physiological and psychological arousal, which cause a higher secretion of cortisol, endorphins, and fibrinogens, that is, substances affecting the level of plasma lipids, blood pressure and coagulability, cardiovascular reactivity, and risk of depression. Chronic exposure to stress has also been found to cause coronary artery atherogenesis and affect the immune response [8]. Finally, stress affects health indirectly due to greater use of stress-relievers such as alcohol, tobacco, and drugs that induce risky social behaviors and reduce a person’s ability to maintain their emotional balance.
An unexpected increase in unemployment appears to have been the most significant stress factor that impacted mortality during the political transition in Europe. Mortality increased the most in countries, districts, and years that recorded adverse labor market changes [3]. These findings confirm the results of quasi-experimental studies of factory closures and follow-up studies of unemployment, which provide evidence of higher mortality due to violent causes as well as circulatory and alcohol-related diseases among the unemployed [3]. When considering the potential pathways through which unemployment affects health, loss of income is the most obvious. However, unemployment also causes loss of skills, cognitive abilities, motivation, sense of confidence, and psychological balance [9]. Additionally, the sense of social exclusion felt by the jobless may cause an increase in domestic violence and crime rates.
A second source of acute stress has been attributed to mounting income inequality, which erodes relations of interpersonal trust and mutual insurance. Unequal societies are afflicted by a high incidence of cardiovascular problems that can be attributed to minimal involvement in community life and personal isolation, see the literature cited in [2]. On the one side, central European economies experienced surges of only four to six points in the Gini coefficient, as they were able to mitigate the fall in gross domestic product and tax revenue that occurred immediately after the transition while also introducing unemployment compensation and social assistance. On the other hand, in the FSU and south-east Europe, the Gini coefficient rose by 0.10−0.20 points while social transfers simultaneously collapsed. Such huge spikes in inequality placed a considerable psychological burden on the losers, namely middle-aged, semi-skilled industrial or collective farms workers and former party cadres. As the new élites often reached their positions through ascription and corruption, the losers experienced feelings of rage and hopelessness. Social disorientation was particularly acute for elderly and middle-aged adults who saw the traditional social values and norms that they had grown accustomed to during their lifetimes vanish overnight.
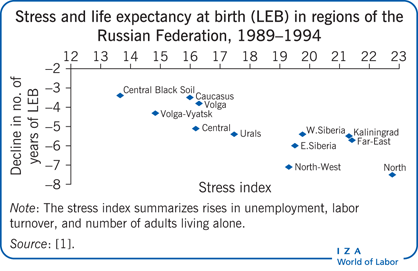
A third significant stressor was family erosion. As noted before, stress-related mortality is highest for adults who are widowed, divorced, and single. During the FSU transition, the number of widows and widowers rose, the crude marriage rate fell by 16−54%, and the divorce rate edged upwards by 10−15%. Although measuring the health impact of these changes poses considerable challenges, regression analysis carried out on the 12 Russian macro-regions over 1989−1994 suggests that a 0.20 point increase in the Gini coefficient led to a reduction in male LEB of 1.5 years, while a 10 point rise in unemployment reduced it by 3.5 years [1]. However, it is important to point out that—also in this study—an important share of the observed decline in LEB remains unexplained.
Limitations and gaps
The efforts of many scholars have shed light on one of the largest peacetime demographic disasters of the 20th century. Though with different emphasis, most authors now agree that the mortality crisis was caused by the acute psychosocial stress that resulted from the upheaval caused by the transition from a planned to a market-based economy and from communism to liberal democracy. A surge in alcohol consumption is also considered a relevant factor, while the weakening of state institutions is seen as an associated factor. Such conclusions are primarily made on the basis of grouped data that only permit conclusions based on weak inference. The impossibility of using micro data, either because it is simply unavailable or because some of the relevant variables (e.g. alcohol prices) are available only in aggregate terms, does not facilitate conclusive testing of the relative importance of stress and alcohol consumption.
Another limitation in the literature concerns the explanation of huge differences in country responses to the mortality crisis. There is not yet an accepted theory for why countries’ responses differed so drastically. Thus, the arguments presented may not be able to capture the deep-seated social and political causes of the crisis. For instance, the limited government response to the shocking mortality rises recorded in the FSU remains incomprehensible and unexplained. The conjecture that those most affected belonged to marginal groups with no “voice” remains untested and could potentially be contradicted by explanations emphasizing the collapse of the state, a weak civil society, or other factors. Thus, the ten million excess deaths recorded in the FSU between 1990 and 2000 still lack an adequate political theorization.
Summary and policy advice
The moderate fall in LEB seen from 1989 to 1991 in central Europe was followed by a quick return to normal mortality levels. In stark contrast, the other post-communist European transition economies experienced an unprecedented fall in LEB that began in 1989 and, for several of those nations, continued well into the 21st century. The Ruble crisis and debt default in 1998−1999 contributed to the mortality crisis in Russia and the former communist countries closely connected to Russia by trade and economic relations. Only after 2005 did such countries record steady LEB gains.
Such disturbing trends resulted, at least in part, from a sharp rise in acute psychosocial stress that has been attributed to unanticipated rises in unemployment, job turnover, job insecurity, income inequality, social stratification, family erosion, and distress migration. In countries that experienced the sharpest rises in death rates, weak institutions and a passive public policy did little to stop deteriorating public health. Indeed, while the mortality crisis was unexpected, its impact was mostly neglected, possibly because it concerned an underclass of poorly educated, unemployed, and single, marginalized people, who had no “voice” in the newly formed political regimes.
The European transition mortality crisis confirms that poorly managed economic upheavals as well as large and sudden societal transformations can generate acute deteriorations in public health. The recent 35% increase in male suicides recorded in Greece during the ongoing economic crisis provides another example of the need to adopt measures to control increasing financial instability, unexpected job loss, and personal insecurity [10]. Swift policy responses to address these issues are required, both for the specific benefits they produce (e.g. better labor market outcomes) and because of their positive impacts on health.
The measures needed under such circumstances include properly paced macroeconomic adjustments and industrial restructuring, job re-training, public works, unemployment compensation, wage subsidies, and measures to contain surges in inequality, social exclusion, family breakdowns, and distress migration. Deaths due to violent causes and infectious diseases can also be avoided by strengthening the social assistance services that deal with people marginalized by crises. A stricter regulation of alcohol consumption and other stress relievers would also help to reduce violent and cardiovascular deaths. To be sure, rigorous market reforms are needed; however, as the Czech Republic and Poland demonstrated in the early 1990s, these reforms must be characterized by a realistic pace of restructuring and strong labor, social sector, and redistributive policies.
Acknowledgments
The author thanks two anonymous referees and the IZA World of Labor editors for many helpful suggestions on earlier drafts. This paper draws, in part, on prior works of the author, and work conducted in collaboration with R. Paniccià [3].
Competing interests
The IZA World of Labor project is committed to the IZA Guiding Principles of Research Integrity. The author declares to have observed these principles
© Giovanni Andrea Cornia