Elevator pitch
Recessions are complex events that affect personal health and behavior via various potentially opposing mechanisms. While recessions are known to have negative effects on mental health and lead to an increase in suicides, it has been proven that they reduce mortality rates. A general health policy agenda in relation to recessions remains ambiguous due to the lack of consistency between different individual- and country-level approaches. However, aggregate regional patterns provide valuable information, and local social planners could use them to design region-specific policy responses to mitigate the negative health effects cause by recessions.
Key findings
Pros
Substantial country-level research shows that mortality declines (i.e. people live longer) during recessions.
Recessions can make more time available for individuals to lead a healthy lifestyle.
Motor vehicle deaths have been shown to decrease during recessions.
Some studies suggest that during recessions the stigma of being unemployed decreases.
Cons
A plethora of individual-level studies show that recessions lead to adverse mental health, especially for working-age and low-income people.
The number of suicides appears to increase during periods of recession.
Income loss due to recessions decreases investments in health-enhancing goods and services.
Austerity measures that may be common during recessions, such as budget cuts to social welfare, mainly affect vulnerable population groups and the long-term unemployed.
Author's main message
Evaluations of the health-related impacts of economic recessions have shown inconsistent results. However, if recessions cause a greater deterioration in individuals’ mental health and a larger number of suicides, then governments should be motivated to work even harder to recover the world’s economies after downturns occur. Governments should acknowledge that the potential impact of recessions on people’s health depends on the extent to which people are protected from vulnerability. Welfare policies, such as labor market programs, debt relief programs, and access to health and mental health services, should thus play a significant role as a mediator in the relationship between recessions and health.
Motivation
Various theories in social epidemiology and health economics suggest that recessions, which are mainly classified as periods of increased unemployment and income loss, are complex events that affect health, mental health, and behavioral patterns through a range of potentially opposing mechanisms [1], [6]. The social epidemiology literature on this topic consists of country- and individual-level research. Country-level studies mainly examine how unemployment affects pathology (i.e. mortality and certain health conditions) [1]. The individual-level research primarily examines how individuals’ increased unemployment and income losses during a recession affect self-reported health, mental health, and health-related behaviors such as alcohol consumption [1]. Focusing on individual-level research, recessions can have adverse health-related consequences; by contrast, country-level studies rely upon a host of theoretical frameworks and a great deal of empirical evidence that suggests the opposite to be true [6]. As such, the overall impact from recessions is hard to predict and may well differ between countries and subgroups within populations [1]. Many country-level studies show a link between increased unemployment and reduced mortality, whereas many individual-level studies find a connection between increased unemployment and mental health deteriorations [2], [7].
To draw general conclusions, aggregated evidence regarding which mechanisms play a role in which context and for which subgroup within a population is needed [7]. Such evidence can help to determine efficient policies that could be implemented during periods of increased unemployment to mitigate (or reverse) the deterioration of people’s health [1]. An understanding of the relationship between recessions and well-being is important for developing effective policies aimed at improving health indicators and decreasing social inequalities [7].
Discussion of pros and cons
Mental health and well-being
In the public health community, concerns are often expressed about the negative mental health consequences associated with recessions. A vast amount of individual-level research has shown that economic recessions can increase anxiety, stress, depression, alcohol and tobacco consumption, and suicides, to list only a few. All of this results from loss of employment, fear of losing one’s job, income reductions, loss of savings, foreclosure, and eviction [7]. In an international review of 237 cross-sectional and 87 longitudinal studies, researchers estimate that unemployed individuals exhibit greater mental health problems than employed individuals [8]. Several international studies conclude that unemployment and/or income loss can result in adverse mental health symptoms because unemployed people are stripped of certain functions of employment, including time activity, a collective purpose structure, goals, physical security, social contact, and status [7]. These findings are strongest among young people and vulnerable population groups [1], [6].
Indeed, unemployment and income loss severely frustrate the human desire for agency and self-directedness [7]. Moreover, the literature suggests that significant acute and chronic stressors are related to changes in physiological regulation that leads to deteriorating health [1], [7]. In addition to this, high-risk lifestyle behaviors, such as smoking and alcohol consumption, typically increase during unemployment and after income loss [7]. The tendency to take up adverse health behavior after job loss is seen as a method of coping with the stress that comes with being stripped of a social role [7]. Moreover, income loss is expected to decrease investments in health-enhancing goods, and can result in both poor physical and mental health [7]. Importantly, during economic recessions, the psychosocial burden of being unemployed can be greater than before due to the fact that increased unemployment reduces people’s chances of finding a new job. This situation puts these individuals at a much greater risk of being trapped in long-term unemployment, which entails greater insecurity, stress, and economic problems. Indeed, all of this can lead to a significant increase in the number of depression incidents [3]. Several recent studies that focus on the Great Recession of 2008 and the EU financial crisis of 2009 verify the aforementioned pattern [3], [4], [7].
During recessions, an increased number of unemployed and low-income people rely more heavily on state health benefits, which tend to receive less support from governments due to contracting national budgets. This reduction in support for critical health services, which can affect both the quality and quantity of services offered, may have severe impacts on unemployed and low-income people’s health [7]. Additionally, insurance companies frequently make changes to their policies on deductibles when recessions occur, lowering the probability that even those individuals who do have coverage will be able to seek timely health and mental health care (to say nothing of the even greater difficulties faced by those who do not have coverage in non-nationalized health systems) [1]. Austerity measures, which reduce public budgets in areas such as health care, combined with greater personal financial struggles due to long-term recessions, may also contribute to poorer health status for the unemployed during economic downturns [7]. Austerity measures such as budget cuts to social welfare and health care mainly affect people with low incomes, low educational levels, and those who are long-term unemployed [7]. The additional burdens imposed on these vulnerable groups due to austerity measures exemplifies the ways in which recessions can affect subgroups within a country in different ways [1]. Moreover, the combination of low income and less financial support may dramatically increase the vicious cycle of psychological distress in lower socio-economic groups [7].
In the international literature, the evidence on how recessions affect individuals’ mental health due to increased unemployment and income loss does not agree on all (or even most) fronts. Some studies suggest that a reduction in time spent at the workplace could reduce the prevalence of work-related stress and allow more time to pursue a healthy lifestyle through better dieting and exercise [2]. Especially for people in stressful professions, becoming unemployed may actually reduce the prevalence of adverse health and mental health-related problems [2]. Thus, recessions may lead to a reduction in the number of existing stressful jobs and their effect on well-being [2], [3], [4], [6]. Individual-level research finds that when unemployment increases under a recession and becomes a more prevalent condition in society, the psychological cost of being unemployed might diminish and the subjective well-being of the unemployed thus improves [2], [7]. However, this pattern might be affected by social protection responses, such as long term unemployment benefits and access to health and mental health services, which are crucial for mitigating living, health, and mental health concerns [7].
Mortality
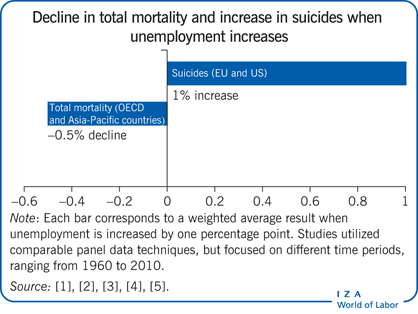
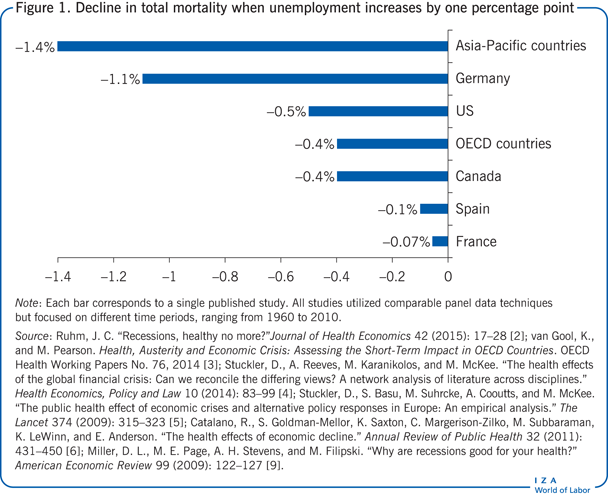
Mortality is the most common proxy for general health status because it represents the most severe health outcome (death); many researchers conclude that mortality rates are the most reliable indicators of a population’s overall health [1]. Substantial country-level research has shown that mortality rates decline when the economy weakens (i.e. people in the affected area seem to live slightly longer during recessions). As seen in Figure 1, studies that use comparable panel data techniques but focus on different time periods, ranging from 1960 to 2010, demonstrate that an increase of one percentage point in the unemployment rate decreases mortality rates by varied amounts, from 0.07% in France to 1.4% in Pacific-Asian countries (including Hong Kong, Japan, South Korea, Malaysia, the Philippines, Singapore, Taiwan, and Thailand) [2], [3], [4], [5], [6], [9]. A few US studies suggest that during economic downturns, reductions in smoking, drinking, obesity, and physical inactivity may occur, which can have a positive effect on mortality rates (i.e. people are healthier overall) [2], [3], [4], [6]. Indeed, a number of medical problems, such as cardiovascular and liver diseases seem to fall in economic recessions, as several US studies show [2], [9].
It is important to note here that some alternative studies, also from the US, suggest that economic growth has been the central factor in the decline in mortality rates during the 20th century [10]. Further complicating the matter, recent studies from the US provide mixed results, implying either a weak negative association or no association between economic hardships and mortality rates [2]. It is also worth considering results from current EU studies, which do not show an effect on cardiovascular diseases from unemployment, but significant associations with unemployment and deaths due to alcohol abuse [5]. Hence, results from the existing literature should not be considered universal; some researchers believe that the relationship between mortality rates and business cycles should be viewed as a time varying phenomenon [2], [5]. Indeed, current EU studies suggest that while the temporary effect of an increase in unemployment is to lower mortality, the permanent effect is to increase it [11]. Moreover, it is probable that mortality rate declines may mask hidden health problems, such as liver and lung diseases, especially for vulnerable population groups, which are disproportionately affected by the adverse effects of economic recessions [1], [7].
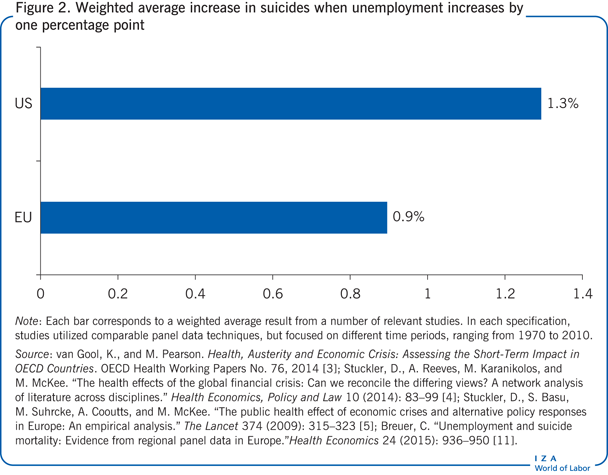
Interestingly, research from the US suggests that motor vehicle deaths decrease during recessions, probably because fewer people commute to work, and/or because people reduce alcohol consumption [2], [9]. However, the same literature suggests a significant relationship between increased unemployment and suicides [2], [3], [4], [9]. As observed in Figure 2, several country-level studies show that a one percentage point increase in the unemployment rate is estimated to increase suicide rates by 0.9% in the EU, and by 1.3% in the US [3], [4], [5], [11]. These patterns become stronger in young population groups (i.e. below the age of 40) [1], [3], [4], [11]. In addition, recent data show that suicide rates in the US and the EU have been on a remarkable upward trend following the Great Recession of 2008 and the EU financial crisis of 2009 [3], [4], [11]. Thus, social living conditions such as unemployment and income are perceived to be rational determinants of suicide behaviors [11].
Alcohol and tobacco consumption
Alcohol and tobacco consumption are shown to be both positively and negatively affected by recessions, with a number of studies disagreeing on this point [1]. Changes in alcohol and tobacco consumption can have a considerable effect on public health, as their levels are causally related to many chronic medical conditions such as cancer and cardiovascular diseases [1], [5], [6]. Alcohol-related behaviors also bring with them substantial negative societal issues, both direct and indirect, including crime, violent behavior, traffic accidents, and social exclusion [1]. Recent studies from the US suggest that a decline in economic resources is associated with an increased risk of smoking and drinking problems [12], [13]. These patterns fit well with EU studies, which suggest that alcohol consumption may increase during spells of higher unemployment [5]. However, these results contradict previous US studies, which indicate that there is a negative relation between recessions and smoking and drinking [2], [9]. These contradicting patterns suggest that the impact of recessions on alcohol consumption might depend on a person’s economic and social situation [1], [3], [4].
Regarding the positive relationship between recessions and substance abuse, increased stress due to a higher risk of becoming unemployed and/or lower incomes may lead to a less healthy lifestyle behavior profile than before recessions [12], [13]. In periods of adverse economic conditions, smokers and drinkers may smoke and drink more because they are more stressed, angry, anxious, sad, and inactive, and believe that smoking and drinking will alleviate these moods and stresses [12], [13]. However, a decrease in working hours will lead to more time for social events and watching television; in turn, these activities might lead to more consumption of alcohol and tobacco [12], [13].
Arguing for a negative relationship between recessions and substance abuse, several scholars have suggested that a lighter workload during economic recessions may lead to less stress and thereby to a reduction in alcohol and tobacco consumption [2], [9]. In addition, during economic recessions, employed people might consume fewer drinks and drink less heavily in order to increase their chances of holding onto their job, while unemployed people lower their consumption in order to increase their chances of getting a new job [2], [9]. Finally, as a result of personal income reductions, tighter budget constraints during a recessionary period could lead to less money being spent on tobacco and alcohol [2], [9]. Having said this, it must be kept in mind that some alternative strategies that drinkers use to adjust to tighter budget constraints are to switch to cheaper alcoholic beverages, or to substitute drinking in bars with drinking at home [3].
Limitations and gaps
It is important to highlight that different methodological approaches could generate different results. For instance, country-level studies find that mortality rates generally decline during economic contractions [1], [3]. By contrast, individual-level studies suggest that unemployment itself leads to poorer mental health and well-being [7]. Although these measures are perceived as reliable health indicators, some researchers suggest that aggregate medical reports would likely provide more robust indicators for evaluation purposes. Self-reported health and mental health studies might reveal biased patterns if individuals present themselves as having more severe health/mental health issues to the interviewer, or the other way round [7]. Such behavior could result in overestimation or underestimation of health issues, respectively.
Consider also that studies on mortality rates alone might fail to capture the complex nature of population health and mental health dynamics, thus resulting in an underestimation of potential effects. For example, country-level studies do not allow for a clear identification of who has been affected, how they have been affected, who has not been affected, or to determine the magnitude of the impact on specific health conditions. In addition, while recessions seem to reduce mortality rates among the population as a whole, they may worsen rates among specific social groups [1], [5], [7]. Thus, varied individual- and country-level settings as well as different health status indicators make drawing general conclusions difficult. A clear understanding of the patterns captured, and not captured, by each study is important when considering potential policy implications.
Crucially, recessions vary in their depth and length, which is likely to influence their impact on health-related problems. Without longitudinal data of sufficient duration and without meta-analyses that control for recession characteristics, it is not possible to assess the direction and significance of the relationships, nor is it possible to offer firm conclusions or comparisons between regions. It is very important to have a clear understanding of the appropriate time lag before any causal conclusions about the relationship between recessions and health status can be drawn. Indeed, the health and mortality consequences from economic recessions could occur after a (significant) time delay. Thus, adverse health consequences resulting from a previous recession might not appear until the recovery phase is already underway. This significant feature would lead to biased patterns found during both the recession and recovery periods.
As the impact of recessions could well differ between subgroups within a country, more work is needed on this issue, as many studies have failed to control for age cohorts, pre-recession health conditions, and low-income groups. Moreover, by considering pre-recession health conditions, researchers could reduce the prevalence of biased results and better clarify causality paths. Controlling for pre-recession health status, and/or splitting samples into healthy vs health-impaired people (according to their statuses before the recession), would make it possible to rule out the chance that health-impairments affect unemployment, inactivity, and reduced income during recessions, but not at other times. In general, it might be that a significant deterioration in health status is observed only among those who were health-impaired before recessions and before the onset of unemployment. It is therefore important to build a well-developed pool of longitudinal data that allows researchers to account for changes in employment and health status over time.
Future research on this topic would benefit most from meta-analyses that could empirically evaluate whether social safety nets are able to minimize the adverse health effects of recessions. Multivariate meta-analyses should control for valuable information such as the recession’s depth and length, pre-recession health status, and age cohorts, so that clarification can be gained about regional differences with respect to health-related outcomes and health policies. In the same vein, meta-analyses should consider controlling for austerity measures, particularly for wage and pension reductions in addition to cuts in health budgets. Indeed, this would help to explain regional differences when it comes to health-related outcomes and austerity measures. These results would allow for the creation of research-led policy proposals designed to minimize the negative impacts of recessions, and maybe even maximize the positive ones. Given the phenomenon’s importance and the potential for research-informed action that could affect people’s health status, this research area cries out for robust future work [7].
Summary and policy advice
Existing evidence on economic recessions and their impacts on people’s health provides no clear-cut conclusions [3], [4], [6], [7]. Some evidence supports the notion—resulting from country-level research—that economic downturns reduce mortality and motor vehicle deaths, but lead to an increase in the number of suicides [3], [4], [6]. Individual-level studies primarily suggest that mental-health indicators deteriorate during recessions [6]. However, it is difficult to reach firm conclusions about the relationship between recessions and certain health problems, such as cardiovascular and liver diseases [3], [4]. The same holds true for the relationship between recessions and tobacco and alcohol consumption [6], [7], [13]. Regional differences, demography, depth and length of the recession, austerity measures, and social welfare programs are factors that probably impact the relationship between economic downturns and health [3], [4], [7].
As general conclusions remain elusive, countries should consider the aggregate patterns emerging from their respective regions and take the relevant actions that are most suited to their specific situation. For example, if regional indicators suggest that people’s health and mental health deteriorate and that tobacco/alcohol consumption increases during recessions, then relevant welfare policies should be implemented in order to minimize these consequences [7]. In addition, if recessions negatively affect working-age people and specific population groups, such as those with lower education and lower income, then enhancing social protection policies for those groups would be appropriate [1]. Labor market programs, together with family support programs, minimum-income benefits, long-term unemployment benefits, debt relief programs, and access to health and mental health services can all be effective ways of preventing or mitigating the adverse effects of recessions on well-being indicators [7].
Presently, while severe recessions are ongoing in many countries, it is more timely than ever to investigate whether specific factors such as individual and family support programs, health campaigns, debt relief programs, provision of unemployment and health benefits, and active labor market programs are able to minimize mental health problems, suicides, mortality, specific health situations, and alcohol and tobacco consumption. If it is proven that social safety-net programs have preserved the health of populations during past recessions, then this feature might be able to partially explain why, in some regions, adverse health problems were not prevalent (or were even reduced) during times of economic decline. In all cases, social planners should acknowledge that the extent to which recessions affect a population’s health depends upon the extent to which people within that population are protected from vulnerability [7].
Acknowledgments
The author thanks two anonymous referees and the IZA World of Labor editors for many helpful suggestions on earlier drafts.
Competing interests
The IZA World of Labor project is committed to the IZA Guiding Principles of Research Integrity. The author declares to have observed these principles.
© Nick Drydakis