Elevator pitch
Research finds that hot weather causes a fall in birth rates nine months later. Evidence suggests that this decline in births is due to hot weather harming reproductive health around the time of conception. Birth rates only partially rebound after the initial decline. Moreover, the rebound shifts births toward summer months, harming infant health by increasing third trimester exposure to hot weather. Worse infant health raises health care costs in the short term as well as reducing labor productivity in the longer term, possibly due to lasting physiological harm from the early life injury.
Key findings
Pros
Hot weather reduces birth rates eight to ten months later, with the largest reduction occurring at nine months.
Decline in births related to high temperatures is likely due to worse reproductive health at conception, not reduced sexual activity.
A modest rebound effect in birth rates occurs 11–13 months after high temperatures, partially offsetting the initial decline in fertility.
Air conditioning may help offset some of the negative effects of hot weather, though it may also exacerbate climate change.
Cons
The impact of hot weather on fertility is less clear in developing countries, where birth rates are typically higher and public health resources are limited.
More research with humans is needed to determine whether the impact on reproductive health is larger for males than females, as is suggested by animal studies.
The rebound in birth rates shifts births to summer months where children will be exposed to dangerous hot weather during the third trimester.
Compared with birth control policy or female labor market participation, temperature is less important for predicting historical changes in fertility or differences in fertility across countries.
Author's main message
Relatively little attention has been paid to how temperature shocks might affect prime-aged adults, especially via their reproductive health. Non-experimental studies find that birth rates fall nine months after the occurrence of hot weather. There is suggestive evidence that the fall in births is due to worse reproductive health and not diminished sexual activity. Providing the public with information regarding this negative link might help people better adapt. Increased use of air conditioning might be one concrete step for adapting, though this response will potentially increase greenhouse gas emissions and climate change.
Motivation
Heatwaves occur relatively frequently and are only likely to increase in regularity with unabated climate change. These climatic shocks pose dangers to public health, and policy intervention could help mitigate the societal costs. Public information campaigns can help individuals better protect themselves from the potential dangers. Direct interventions (e.g. providing access to air conditioned facilities) could reduce the risk to vulnerable populations who are less capable of adapting on their own. For policy efforts to be effective, researchers must first identify the ways in which hot weather influences human health and welfare. The link between temperature and fertility is deserving of attention for two reasons. First, total completed fertility affects family welfare and funding for social insurance programs, such as Social Security in the US. Second, fertility timing (independent of total completed fertility) can affect both short- and long-term health as this will affect the resources available to the child during the critical in utero phase. For example, timing could affect nutritional intake, exposure to pollution, and ambient temperature during certain trimesters.
There are a priori reasons to believe that hot weather would hinder human fertility. Randomized experiments with cattle and mice suggest a causal link between hot weather and worse reproductive health [2]. There is less convincing evidence for humans, though the link between ambient temperature and sperm production is quite plausible given the documented finding that human testes are sensitive to heat [3]. Temperature could also influence fertility via sexual activity through a variety of mechanisms, such as changes in socialization with potential sexual partners. However, the existing evidence on temperature and sexual activity is inconclusive. Studies find that sexual activity follows seasonal patterns, but this may have more to do with holidays than climatic factors [4], [5].
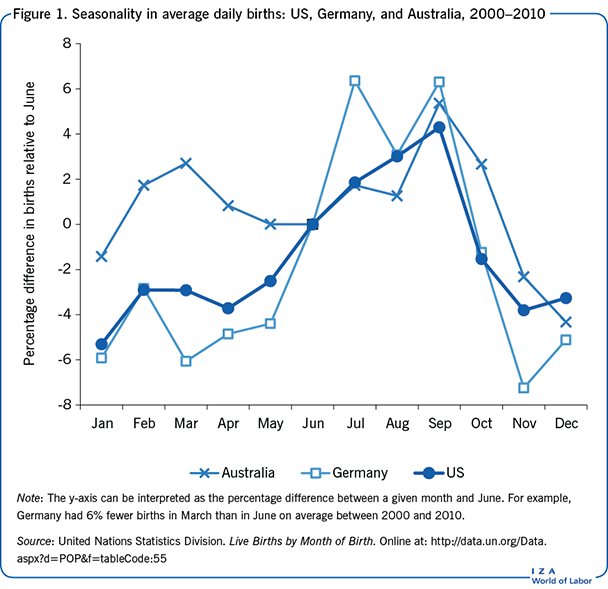
The strong seasonality in birth rates across many countries suggests climatic conditions may have a meaningful impact on fertility. Figure 1 plots the log of total births by calendar month for the US, Germany, and Australia for the years 2000 through 2010 using data from the United Nations. All three countries exhibit a peak in births between July and September, which is summer for the US and Germany, but not Australia. However, Australia also experiences a secondary peak during its summer, around March. This is suggestive evidence that temperature is an important, though not singular, determinant of birth rates.
There are many factors, in addition to temperature, that could explain the birth rate seasonality seen in Figure 1. For example, sunlight, nutrition, school term, employment, disease prevalence, and income all tend to vary seasonally in ways that might be correlated with temperature. Numerous studies explore the various determinants of birth seasonality [6]. There is, however, little consensus on the relative importance of any one of these factors. This article does not discount the importance of other seasonal factors, but chooses to focus on the independent role of temperature given its relevance to climate change.
The focus here is on studies that estimate the effects of temperature shocks since this approach helps isolate temperature from other factors. In simple terms, the studies examine whether there are atypical changes in birth rates following unusually warm months. For example, an unusually hot August in New York may affect birth rates the following May (nine months later). With enough data, the empirical model can also control for secular trends in birth rates (e.g. due to changes in family size preferences), which might be spuriously related to gradual climatic changes.
One important consideration is whether populations can adapt to temperature shocks by shifting conception months. This shift could occur naturally, say, as couples that fail to conceive in one month could simply continue to engage in unprotected sex in subsequent months. Alternatively, the shift could be due to individuals concertedly putting off engaging in physical activity, such as sex, during uncomfortably hot weather. Without accounting for this shift in conception month, the impact of temperature on total completed fertility would likely be overstated. Furthermore, total completed fertility is an important metric in countries where low birth rates and aging populations are putting a strain on social insurance programs. Other forms of adaptation might occur both in the short term (e.g. increased use of air conditioning) and the long term (e.g. migration). Empirical studies implicitly account for short-term adaptations in their analysis, but longer-term adaptations are hard to quantify due to the difficulty in controlling for secular trends towards having fewer children.
In addition to impacting total completed fertility, a shift in conception timing in and of itself could have important social costs. Delaying conception could mean that a birth takes place at a time that is sub-optimal for infant health. Even a shift of a few months could be important since this would alter seasonal conditions (e.g. nutrition, sunlight, pollution, weather, parental income) during particular phases of the pregnancy. Moreover, harm during critical pregnancy phases can have both short- and long-term societal costs. In the short term, sicker infants may require more health care, straining public health systems and possibly increasing the parents’ opportunity cost of working. In the long term, these infants may have lower labor productivity as adults due to lasting physiological harm from the early life injury [7].
Discussion of pros and cons
The initial decline in births approximately nine months later
Using data from the US, two early studies demonstrate that higher temperatures reduce birth rates approximately nine months later [8], [9]. Another US study extends the work of these earlier studies and makes some modeling innovations [1]. The first US study estimates the effect of monthly temperatures on the birth rate nine months later, but only over the relatively small time period between 1950 and 1960 [8]. The study compares atypical temperatures with atypical birth rates to help isolate the causal effects from other factors that vary seasonally in a typical (or expected) way, like school holidays. The data are organized by state and month. In simple terms, the data average all the temperature readings across New York in a given month and compare those temperatures with the birth rate in New York nine months later. The study focuses only on summer temperatures to address the fact that increases in temperature may have a different effect depending on the reference temperature. For example, in the summer, when it is already warm, an increase in temperature may have a negative effect on birth rates. By contrast, an increase in temperature during the winter, when it is cold, may have a positive effect on birth rates.
Furthermore, the model is estimated separately for each US state. As such, the study accounts for potentially different responses to temperature shocks that might occur across states. For example, states that are usually hot may better adapt to temperature shocks, e.g. due to differences in how homes are constructed. However, estimating the model separately for each state reduces statistical power, which limits its informative value. Also, there are nearly 50 sets of estimates, so summarizing the basic findings is difficult. Nonetheless, for many states, the study finds that a 1°C (2°F) increase in summer temperatures causes a 1% decline in birth rates nine months later.
Another study follows a similar approach, but examines the much more expansive time period between 1942 and 1988 [9]. Again, the focus is on atypical temperatures and atypical birth rates to better isolate causal links between the two. Similar to the earlier study, the data are organized by state and month and their model is estimated separately for each state. However, the authors estimate the effects of temperature for white birth rates and non-white birth rates separately, in an implicit attempt to gauge the importance of socio-economic conditions as a modifying factor. They include all months in the analysis instead of focusing only on summer temperatures. Moreover, the authors allow for the possibility that temperature affects the birth rate both nine and ten months later (as opposed to only nine months later).
Despite these changes, this study’s findings are generally consistent with the previous one. For Georgia, the authors find that an increase in one month’s temperature from 24°C to 25°C (75°F to 77°F) would result in close to 1% fewer births nine months later for the white population. The estimate for non-white births is almost half the magnitude for white births in Georgia, though the differences by race are not consistent across all states. In Louisiana, for example, the effect of an increase in temperature from 24°C to 25°C is approximately 1.3% for both the white and non-white populations. The study also finds that hot weather causes a relatively modest reduction in births ten months later.
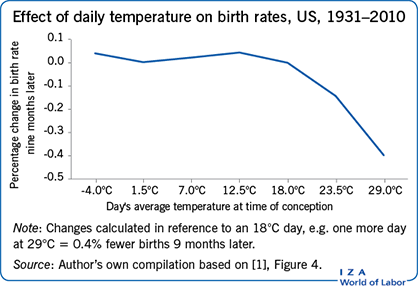
The third study mentioned above also explores the relationship between temperature and fertility in the US, but over the time period between 1931 and 2010 [1]. The data are also organized by state and month. Births of all races are combined in the main model, though the study also estimates the impacts separately by race. The model deals with temperature extremes better than the previous studies by exploring the full distribution of daily temperatures within a month (while the other two studies both averaged the temperature over the entire month). Indeed, the study finds that there is an important “tipping point” when the average daily temperature passes 20°C (68°F). That is, temperature changes below 20°C have little effect on birth rates nine months later. But, as temperature increases past 20°c, there is a dramatic fall in birth rates. For example, one additional “hot day” (above 27°C/80°F) relative to one “mild day” (at 20°C/68°F) causes the birth rate nine months later to fall by 0.4%, or about 1,200 births, in the US.
The rebound in births and effect in other months
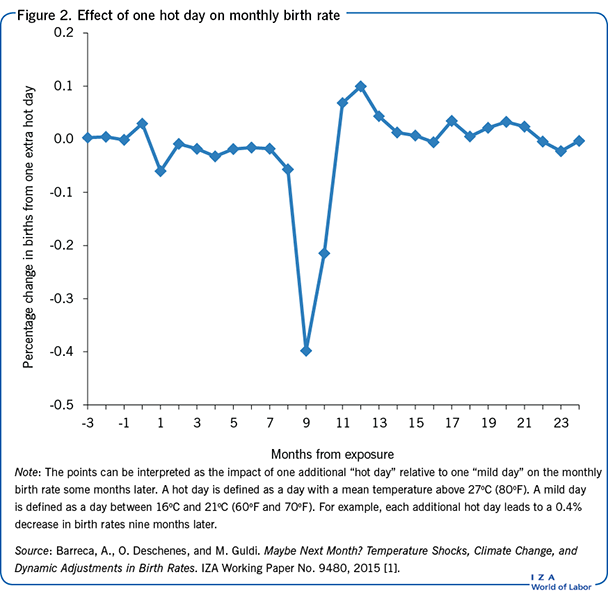
The model in the study just discussed [1], unlike the previous studies, comprehensively tests for a “rebound” in births in the months following the initial decline in births. That is, individuals may be unsuccessful conceiving during a hot month, and simply continue trying during the following month(s). The study shows that birth rates do rebound after the initial decline. Figure 2 plots the effect of one hot day on birth rates some months later. As can be seen, one hot day has a negative effect on births eight to ten months later, with the largest decline occurring at month nine as would be expected if the critical exposure period is around the time of conception.
The estimated effect of temperature for months 11 to 13 is positive, implying that a portion of conceptions likely shifted to later months. The rebound in months 11 to 13 offsets about one-third of the initial decline in births.
There is evidence that exposure to high temperatures leads to premature delivery for pregnancies that are near delivery. As illustrated in Figure 2, high temperatures cause an immediate increase in births at month 0 (the current month) but a reduction in births at month 1 (one month later). The reduction in birth rates in months 2 through 8 might be indicative of fetal losses. The study also tests the validity of the model by showing that temperatures occurring after the births have no effect (i.e. months -3, -2, and -1). In other words, there is no plausible way that this month’s birth rate could affect whether the next few months will be hotter than usual.
Moreover, these estimates can explain much of the seasonality in births in the US. As illustrated in Figure 1, a dip in births is observed in the spring months, and an increase is seen in the summer months. This implies that hot summer weather would cause births to decline the following spring, and the shift in time of conception would cause a slight increase in births the following summer. As one metric of the model’s explanatory power, the study examines the “variance” in births across calendar months. The variance is defined as the square of the difference between (i) actual births for a given calendar month, and (ii) the expected average if births were constant throughout the year. When accounting for the “rebound,” the model predictions explain half of the variance in birth seasonality in the US [1]. When neglecting the rebound, the model predictions only explain one-quarter of the variance. While temperature is strongly predictive, half the variance remains unexplained, suggesting that other factors (e.g. school holidays) still may be important determinants of birth seasonality [6].
There is empirical evidence that the shift in births from the spring to the summer will carry both short- and long-term costs. In particular, the shift will cause infants in utero to experience more hot days during the third trimester. In the short term, this will lead to worse infant health. One study finds that each additional hot day during the third trimester reduces birth weight, which is a good proxy for the general health of the infant [10]. The extent to which this translates into additional health care costs remains an open empirical question. In the long term, third trimester exposure to high temperatures may also reduce labor productivity into adulthood, possibly due to lasting physiological harm caused by the early life injury. Recent work finds that hot weather in the third trimester leads to lower annual earnings some 30 years later, though the magnitude of the effect is only modest [11].
Reproductive health
Understanding the particular cause of the decline in births some nine to ten months later can help inform a more effective policy response. Hypothetically, the decline in births could be due to worse reproductive health, for males and/or females, or because of diminished sexual activity. There is suggestive evidence that the initial decline in births is due to worse reproductive health about two weeks prior to conception. This conclusion can be inferred from the fact that hot days not only cause births to fall nine months later, but cause a sizable fall in births ten months later as well. If the critical impact occurred around conception, say, causing a reduction in sexual activity, then one would expect little or no decline in births ten months later since nearly all pregnancies span nine months or less from the time of conception. As noted in Figure 2, the effect of one hot day at month ten is approximately half the size of the effect at month nine. This rather large decline in births ten months later suggests that temperature has a slightly delayed effect on conception chances. This is most easily explained by temperature having a lasting effect on reproductive health as opposed to a delayed effect on sexual activity.
Though reproductive health is the likely channel, it is unclear whether any policy response should prioritize protecting males or females. On the male side, it is well documented in randomized experiments on animals that hot temperatures diminish sperm production [2]. On the female side, animal studies suggest that exposure to hot weather may affect the development of the fertilized embryo, but impacts on fertilization are less clear [2]. While these animal studies point towards males’ reproductive health at conception being more sensitive to temperature, the extent to which this applies to humans is unclear given the lack of evidence. More research with humans, both experimental and observational, is needed to determine the differential effects of hot weather by gender.
The role of air conditioning
It has been shown that the effects of temperature are smaller in states that are accustomed to higher temperatures [1]. Further analysis indicates that the effects of hot days declined considerably following the adoption of air conditioning. The effect of one hot day halved between the 1950s and the 2000s, roughly the same period in which residential air conditioning ownership increased across the US. Each hot day caused the birth rate nine months later to fall by 0.6% during the 1950s, but only by 0.2% during the 2000s. Air conditioning coverage in the US increased from almost no one having it in the early 1950s to over 80% by the 2000s. This suggests that policies aimed at increasing access to air conditioning may help mitigate the fertility costs of hot weather. However, increased air conditioning usage will lead to more energy consumption and greater green house gas (GHG) emissions, which will only lead to greater climate change. Thus, such policies should also consider reductions in energy usage elsewhere in the economy or improvements in energy efficiency (“green energy”).
Limitations and gaps
There are several limitations to the existing studies and important gaps in the current knowledge base on this subject. First, temperature is not a singular determinant of fertility. In a historical context, the estimated effect of hot weather is modest. For example, birth rates fell by 50% in the US between the 1970s and 2000s, due in part to changes in birth control access and labor market opportunities for women [12]. Comparatively, the finding that one hot day reduces birth rates nine months later by approximately 0.4% is quite small. Relatedly, differences across countries are potentially driven more by economic and social factors than climatic ones. As such, the fact that hot developing countries have higher birth rates does not refute the findings from the above-mentioned studies that hot weather reduces fertility.
Second, assessing the impact of climate change (as opposed to weather) on birth rates is difficult without making very strong assumptions. The temperature/fertility studies mentioned above do not capture long-term adaptations or structural changes in the economy, which might occur with climate change. Gradual climatic changes could affect food systems, migration, and economic policies, among other things. And these “other factors” could influence fertility in both positive and negative ways.
Finally, the existing research focuses almost exclusively on the US. More research is needed to assess the validity of the results in other country contexts, as a decline in total completed fertility due to hot weather will have different social costs across countries. In particular, the impact of hot weather on fertility in developing countries is less clear. For developing countries, high fertility rates may strain public resources, so a decline in total completed fertility may improve financial conditions, though it could still negatively affect people’s ability to have the family size that is right for them. Furthermore, many developing countries are located in warm tropical climates, which are likely to experience even greater costs of climate change because of the disproportionate increase in the frequency of extremely hot weather.
Summary and policy advice
Research suggests that hot weather imposes fertility costs by reducing the number of births nine months later. There is only a partial rebound in births in the few months after the initial decline, suggesting that the hot weather still reduces total completed fertility. The potential reduction in completed fertility adversely affects developed countries with low fertility rates and an aging population, since the working-age population funds social insurance programs. The rebound in births shifts more births to the summer months, which harms infant health due to increased exposure to hot weather during the third trimester. Worse infant health carries both short- and long-term social costs. In the short term, unhealthier infants may require additional health care. In the longer term, these infants are likely to have worse health and earnings potential, possibly due to lasting physiological damage from the early life injury.
There are two practical policy responses to mitigate the effects of hot weather on fertility. First, information campaigns could help warn the public of the potential dangers to reproductive health from exposure to hot weather. This would help motivate individuals to protect themselves, e.g. by using more air conditioning. Second, providing air conditioning in public spaces could mitigate fertility costs for populations who do not have the capacity to self-protect (e.g. low-income individuals). However, relying on air conditioning as an adaptation strategy may end up exacerbating climate change by increasing energy use and GHG emissions. Thus, the use of air conditioning should be offset with improvements in energy efficiency and reductions in GHG emissions in other sectors of the economy where the costs are not as great as those on fertility.
Acknowledgments
The author thanks three anonymous referees and the IZA World of Labor editors for many helpful suggestions on earlier drafts. Previous work of the author contains a larger number of background references for the material presented here and has been used intensively in all major parts of this article [1].
Competing interests
The IZA World of Labor project is committed to the IZA Guiding Principles of Research Integrity. The author declares to have observed these principles.
© Alan Barreca
Gestational length
Sources: Fehring, R. J., M. Schneider, and K. Raviele. “Variability in the phases of the menstrual cycle.” Journal of Obstetric, Gynecologic, & Neonatal Nursing 35:3 (2006): 376–384; Wilcox, A. J., C. R. Weinberg, and D. D. Baird. “Timing of sexual intercourse in relation to ovulation.” New England Journal of Medicine 333:23 (1995): 1517–1521.