Elevator pitch
Ample empirical evidence links adverse conditions during early childhood (the period from conception to age five) to worse health outcomes and lower academic achievement in adulthood. Can early-life medical care and public health interventions ameliorate these effects? Recent research suggests that both types of interventions may benefit not only child health but also long-term educational outcomes. In addition, early-life medical interventions may improve the educational outcomes of siblings. These findings can be used to design policies that improve long-term outcomes and reduce economic inequality.
Key findings
Pros
An array of medical treatments and public health interventions provided during early childhood results in better health in childhood and adulthood.
Early-life medical treatments and public health interventions improve academic achievement later in life.
At-risk children especially benefit from these interventions, which may reduce inequality.
The benefits of early-life interventions seem to extend to siblings as well.
It may be more productive to shift the policy discussion from increasing the number of prenatal visits to improving the quality of prenatal care.
Cons
For low-risk children, the evidence on the benefits of early-life medical interventions is mixed.
While certain public health interventions have well-documented health returns, little is known about their impact on human capital accumulation.
More research is needed to understand the causal pathways leading to the positive gains from early-life interventions.
Studies relying on sibling fixed-effects may under- or overestimate the causal impact if the effects of early-life interventions spill over to the siblings of treated children.
Author's main message
Early-childhood medical treatments and public health programs improve children’s lives and reduce child mortality. While the evidence is convincing that interventions lead to better health outcomes and to improved academic achievement later in life for at-risk children, the evidence is mixed on the impact on low-risk children. Policymakers should carefully consider potential differences in responses to public health programs across population groups when designing such interventions. Because siblings who are not directly exposed to these interventions may also benefit from them, policymakers should also take such spillovers into account.
Motivation
A large body of empirical research shows that adverse conditions (such as poor nutrition, illness, in-utero alcohol exposure, iodine deficiency, major injuries or mother’s bad health, and psychological stress) during early childhood (the period from conception to age five) have long lasting negative effects on human capital accumulation and economic outcomes as well as on adult health. However, it is unclear whether these negative consequences can be alleviated or eliminated through medical care and public health programs aimed at improving prenatal and early-childhood health.
This is an important question from a public policy perspective and is the focus of this review. An overview of the findings in the literature linking early-childhood health to academic achievement is followed by a discussion of the research on the effects of early-life medical care and public health policies on the human capital accumulation of children. Because of the stark differences in the organization and delivery of health care between developed and developing countries, the focus is limited to studies on developed countries.
Discussion of pros and cons
Early-childhood health and human capital accumulation
The so-called “fetal origins” hypothesis, put forward by epidemiologist David J. Barker in the early 1990s, posits that the origins of many chronic degenerative adult health problems (such as type 2 diabetes and cardiovascular disease) can be traced to in-utero conditions, in particular to inadequate nutrition. Subsequent theories emphasize the impact of early-life postnatal conditions, as well as the in-utero environment, in shaping long-term outcomes. In economics, James Heckman and colleagues formalized this idea in a model that incorporates dynamic complementarities between inputs across different stages of life, showing how skills acquired early in life increase the productivity of investments later on.
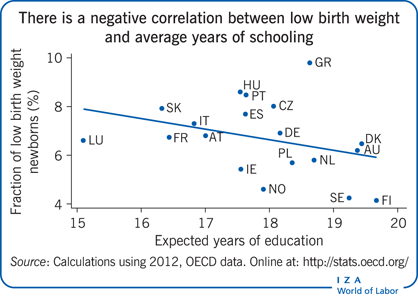
Studies linking early-childhood health to educational outcomes can be classified into two groups: those focusing on prenatal health and those focusing on early-childhood postnatal health. The literature investigating the impact of prenatal health on human capital accumulation generally follows one of two approaches. In one line of work, researchers use birthweight as a proxy measure of prenatal health and examine the impact of birth weight on academic achievement later in life. Most of these studies exploit longitudinal data and employ twin or sibling fixed-effects strategies. Comparing two siblings born to the same mother allows researchers to account for potentially unobserved time-invariant family characteristics that may jointly determine prenatal health and child academic achievement. Results from these studies, based on data from various periods and countries, consistently show a positive association between birth weight and an array of educational outcomes, such as test scores and educational attainment.
A second line of research exploits natural experiments to analyze the impact on human capital accumulation of in-utero exposure to adverse prenatal conditions. Most of these studies employ difference-in-differences estimation strategies and use variation in intensity of exposure to compare the outcomes of cohorts exposed to the “intervention” in-utero to the outcomes of unexposed cohorts. The majority of early empirical evidence on this topic focuses on extreme events, such as famines, influenza epidemics, and radiation fallout from Chernobyl, but recent evidence shows that less extreme events (such as grief and seasonal flu) may also have significant long-term consequences.
Research into the effects of early-childhood postnatal health on academic achievement relies mainly on cross-sectional ordinary least squares or sibling fixed-effects strategies. Some of these studies rely on adult height as a summary measure of early-childhood postnatal health, noting that height during adulthood is strongly correlated with height during early childhood (for example, height at age five) and that height in early childhood is, in turn, affected by prenatal health, poor nutrition, and illness. Several other studies examine how the presence of specific health conditions in early childhood affect human capital accumulation later in life. These studies focus not only on the role of physical health problems (such as asthma and major injuries) but also on the role of mental health issues (such as conduct disorders and attention deficit hyperactivity disorder). The findings from this literature generally indicate that physical illness during postnatal early childhood has less of an impact on academic achievement than fetal exposure to adverse events. However, mental health conditions seem to have large and persistent effects, even after controlling for child health at birth.
Finally, it is worth noting that a growing body of research investigates the impact of parental health during early childhood on the human capital accumulation of children. While this is a relatively understudied topic, emerging evidence indicates that parental health (in addition to child health) may be influential in shaping the educational outcomes of children.
Medical care, early-childhood health, and human capital accumulation
The WHO, whose guidelines recommend 12–16 prenatal care visits for pregnant women, reports that more than 98% of pregnant women in developed countries have at least one prenatal health care visit. Most economic studies in this area focus on the impact of the number of prenatal care visits on child health at birth, as captured by birth weight. The empirical evidence from studies using randomized trials or exploiting natural experiments generally indicates that the number of prenatal care visits has little effect on birth weight. For example, a study that exploits the 1992 Port Authority Transit strike in Pennsylvania as an exogenous source of variation in the number of prenatal care visits received by low-income mothers, who mostly rely on public transportation to access prenatal care, finds no relationship between the number of prenatal care visits and birth weight [1]. However, the results also suggest that the treatment effects may differ according to the time of the intervention, with visits lost early in the pregnancy having a negative impact on birth outcomes while visits lost late in the pregnancy having little effect.
Consistent with this finding, a recent study finds that longer in-utero exposure to favorable prenatal conditions leads to better educational achievement [2]. The study uses the sudden immigration of Ethiopian Jews to Israel as an exogenous source of variation in the duration of higher-quality prenatal care, including the provision of micronutrient supplements (iodine, iron, folic acid) and improved prenatal medical care technologies. Comparing children who were exposed to the change in prenatal care at different gestational ages, the study finds that earlier exposure to better prenatal care results in higher educational attainment (lower grade repetition, lower dropout rates, and higher baccalaureate rates).
On postnatal medical care, there is robust evidence that early-life medical treatments provided to at-risk children have substantial effects on early-childhood health. One study investigates the impact of the length of the postpartum hospital stay on readmission rates [3]. To address the endogeneity in length of stay, the study exploits changes in federal and state laws that substantially reduced early hospital discharges. The results suggest that legislation-induced increases in postpartum stays reduced hospital readmissions among those with the greatest likelihood of a readmission.
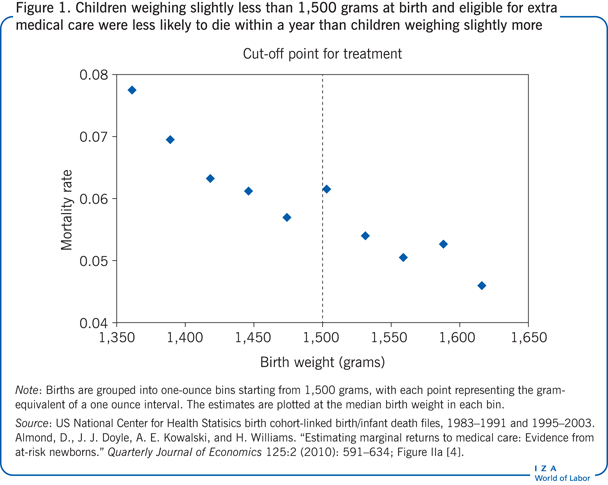
Another US study uses a unique natural experiment to identify the effects of early-life medical treatments on infant health [4]. The study exploits the fact that medical guidelines recommend providing additional treatments to children with a very low birth weight (birth weight below 1,500 grams). Using a design that exploits changes in medical treatments across the very low birth weight threshold, the study finds that children who weighed slightly less than 1,500 grams (and who were thus eligible to receive extra medical care) were less likely to die within the first year of life than children who weighed slightly more than 1,500 grams (Figure 1).
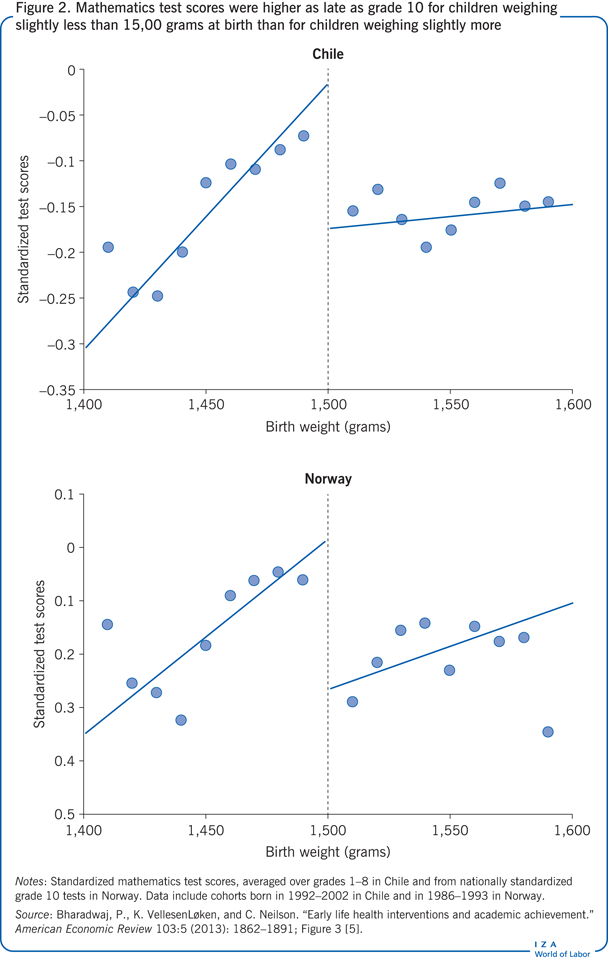
Subsequent work shows that these early-life medical treatments also have significant effects on human capital accumulation. Two recent studies employ a similar methodological design, exploiting changes in medical treatments across the very low birth weight threshold. Using administrative data from Chile and Norway, one study finds that children who were eligible to receive extra medical care at birth had 0.15–0.22 standard deviation higher test scores as late as tenth grade (Figure 2) [5]. The other study uses administrative data from Denmark and confirms that children who weighed slightly less than 1,500 grams at birth (and thus were eligible to receive extra medical care) had higher ninth grade mathematics test scores than children who weighed slightly more than 1,500 grams [6]. The study also documents economically significant spillover effects on the academic achievement of siblings. The estimates suggest that siblings of children who were eligible to receive extra medical care had higher ninth grade language test scores (0.31 standard deviations higher) and mathematics scores (0.36 standard deviations) than siblings of children who were not eligible for extra medical care.
For low-risk children (i.e. children without known medical risk factors), however, evidence on the health impact of early-life medical care is mixed. One study investigates how length of postpartum hospital stay affects infant outcomes among low-risk mothers (i.e. women without known medical risk factors) [7]. The study exploits the fact that insurance rules count the number of midnights in care when reimbursing a predetermined number of “days” in the hospital. Thus, a newborn delivered slightly after midnight has an additional night of reimbursable care compared with an infant born slightly before midnight. The study finds that while infants born just after midnight have significantly longer postpartum hospital stays than infants born just before midnight, both groups of infants have similar health outcomes, as measured by readmission and mortality rates.
Another study of low-risk children uses administrative data from the Netherlands to investigate the impact of home births on the short-term health of low-risk newborns [8]. In the Netherlands, maternity care is provided according to a rigorous process of risk selection based on medical history and current health status, as well as the development progress of the mother and the fetus. To account for non-random selection into a home birth, the study uses a strategy that exploits the variation in distance from a mother’s residence to the closest hospital with an obstetric ward because women who live closer to such a hospital are less likely to give birth at home. The results suggest that giving birth in a hospital leads to significant reductions in infant mortality among low-risk mothers but that the results are driven mainly by the poorer segment of the Dutch population. At this point, there is no research on the effects of early-life medical care on the human capital accumulation of low-risk children.
Public health interventions, early-childhood health, and human capital accumulation
There is robust evidence that public health interventions aimed at improving the early-childhood disease environment can have significant effects on long-term human capital accumulation. A study on the impact of a campaign in the southern US to eradicate hookworm (an intestinal parasite that absorbs nutrients from the blood stream, causing lethargy and anemia) exploits the geographic variation in the prevalence of infection rates [9]. The study finds that school enrollment, attendance, and literacy rates increased after the intervention in areas with higher disease prevalence before the intervention. Following a similar identification strategy, another study finds that malaria-eradication campaigns in Brazil, Colombia, Mexico, and the US led to higher literacy rates and higher income in adulthood [10].
Public health policies targeting early-childhood nutritional well-being may also have significant benefits for health and academic achievement. A notable public health program of this kind is the Special Supplemental Program for Women, Infants, and Children in the US. The program, which covers low-income pregnant and lactating women and children up to age five, provides monthly food checks or electronic benefit transfer cards that participants can use to buy nutritious foods. In addition, participants receive nutrition education and breastfeeding support. A large literature in economics, using a variety of estimation techniques, shows that the program improves infant health at birth, such as birth weight. However, there is almost no evidence on the longer-term health effects of the program and virtually no studies on its impact on human capital accumulation.
There are, however, other studies that document educational benefits for public policies with a nutritional component. For example, one study examines the long-term effects of in-utero alcohol exposure [11]. The study exploits a policy in place in certain regions of Sweden that temporarily allowed individuals younger than 21 to drink strong beer. Children born to women who resided in these regions while pregnant and under 21 at the time the policy was in effect had significantly lower educational attainment, as well as lower cognitive and non-cognitive ability.
Another study investigates the impact of salt iodization on cognitive outcomes in the US [12]. Iodine deficiency is the leading cause of preventable intellectual disability. The identification strategy exploits the introduction of iodized salt in 1924, with the intention of reducing the goiter rate. Before iodization of salt, goiter prevalence varied across regions according to the iodine content of the soil and water. Using this variation, along with the introduction of iodized salt and military data collected during World Wars I and II, the study finds that people born after the introduction of iodized salt in locations with low levels of environmental iodine had larger IQ gains than those born in locations with high levels of environmental iodine. The estimates suggest that the intervention raised the IQ levels of those in the highest quartile of iodine deficiency by almost one standard deviation.
Finally, there is some emerging evidence pointing to human capital benefits for home-visit programs, which are highly popular in developed countries. While the specifics of the programs vary, they generally provide education on parenting skills, infant safety, health, nutrition, and child development. The findings indicate that home-visit programs provided by qualified nurses improve short-term infant health indicators, such as infant mortality rates. Some recent work investigates the impact of well-child visits (visits providing physical examination as well as information on child development, safety, health, and nutrition) on educational outcomes [13]. The study uses a strategy that exploits the differential timing of rollout across Norwegian municipalities by comparing the change in outcomes between municipalities with the program and those without it. It finds that access to well-child visits during the first year of life increases completed years of schooling by 0.12–0.18 years.
Limitations and gaps
There are several limitations and gaps in the work evaluating the impact of early-life medical care and policy interventions. The evidence on the effects of prenatal care comes entirely from studies focused on the number of prenatal visits, and these studies investigate mainly short-term health outcomes. However, because prenatal medical care coverage in developed countries is nearly universal, the quality of prenatal care may matter more than its quantity. In addition, prenatal care may improve outcomes that cannot be captured with readily available proxies of health at birth, such as birth weight. Furthermore, it is possible that certain subpopulations may benefit more from good quality prenatal care than others. More research is needed to fully assess the effects of prenatal care, especially with respect to differences in efficacy of treatments across population groups.
There is robust evidence on the benefits of early-life medical treatment for high-risk children. While these studies have high internal validity (confidence that a causal study has been well done), their results are generally applicable only to “compliers,” individuals whose receipt of medical treatments is determined by the particular instrumental variable exploited by the study. The marginal individual (those who receive medical treatments because of the instrument) in this case may not be representative of the general population. A careful understanding of the external validity (generalizability) of these results is needed when crafting related public policies.
Further research is also needed to reconcile the mixed evidence on the health returns to early-life medical interventions for low-risk individuals. Why do certain types of medical care have higher returns than others? Do medical interventions provide the same health benefits across all subpopulations? What is the role of risk selection in explaining the different findings? Is risk selection always possible? In addition, research is needed to investigate the impact of these interventions on long-term health. Even if there are no effects on short-term mortality, there may be effects on health that become more apparent in the long term. Similarly, more information is needed on the human capital effects of treatments that conclusively provide health benefits.
While there is abundant evidence on the short-term health benefits of the Special Supplemental Program for Women, Infants, and Children in the US, there is limited information on how the program affects postnatal early-childhood health and virtually no information on its impact on longer-term academic achievement. Similarly, there is very little information on how home-visit programs affect long-term outcomes.
Another area where more work is needed is on the impact of medical care and public health interventions targeting parental health (especially during the early life of their children) on the outcomes of children. An emerging literature links poor parental health to worse academic achievement of children. Little is known, however, about whether these adverse effects can be overcome by medical treatments or public health interventions.
More research is also needed to understand the causal pathways leading to the returns to medical care and public interventions, as well as potential externalities generated by the interventions. The net effect of any intervention or treatment depends in part on how parents respond to it. For example, to the extent that parents compensate for differences in early-life health status of siblings, any health improvement due to medical treatments may be offset by reduced parental investments. There is a large body of research on how parents change the allocation of resources within the household in response to these “endowments at birth.” Results from this literature are mixed, supporting both compensating as well as reinforcing behavior depending on the context. However, there is no study in the context of a developed country that specifically considers the impact of early-life interventions on parental behavior.
Finally, it is important to investigate whether medical treatments and public health interventions lead to spillovers within the family. Recent research finds evidence of positive spillovers from some medical interventions to the siblings of treated children. More evidence is needed on the existence of such spillover effects in other contexts. In addition, research is needed to shed light on the causal pathways leading to these spillover effects. These types of information are crucial in interpreting the findings from studies that rely on sibling fixed-effects. If medical care or public health interventions change resource allocations within the household, studies employing sibling fixed-effects may under- or overestimate the true impact of these treatments.
Summary and policy advice
The evidence on early-childhood interventions indicates that various medical treatments and public health programs (especially those for high-risk children) produce not only health benefits but also improvements in long-term educational outcomes. These long-term effects should be kept in mind when considering the cost-effectiveness of any given intervention.
Not all interventions are universally beneficial, however. There is mixed evidence on the returns to early-childhood interventions for low-risk children, implying a potential for cost-savings. Policymakers should take this into account when crafting policies, particularly those targeting large populations, where there may be more scope for differences in treatment efficacy.
Finally, results also suggest that we may have hit the flat part of the curve for some medical treatments. For example, it may be more productive to shift the policy discussion from increasing the number of prenatal visits to improving the quality of prenatal care.
Acknowledgments
The author thanks two anonymous referees and the IZA World of Labor editors for many helpful suggestions on earlier drafts.
Competing interests
The IZA World of Labor project is committed to the IZA Guiding Principles of Research Integrity. The author declares to have observed these principles.
© N. Meltem Daysal