Elevator pitch
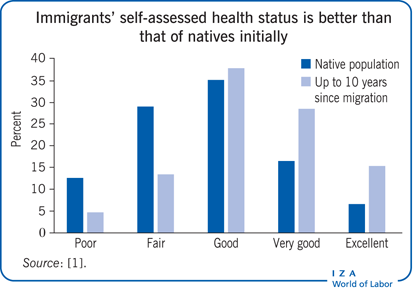
In common anti-immigrant rhetoric, concerns are raised that immigrants bring diseases with them to the host country that threaten the health of the resident population. In reality, extensive empirical research over several decades and across multiple regions and host countries has documented that when immigrants arrive in the host country they are healthier than native residents, a phenomenon termed the “healthy immigrant effect.” This initial advantage deteriorates with time spent in the host country, however, and immigrants’ health status converges toward (or below) that of native residents.
Key findings
Pros
On arrival, immigrants are healthier than native residents (the “healthy immigrant effect”).
New immigrants bring healthier habits and lifestyles, such as physical activity, low-calorie diets, close family ties, and protective cultural factors.
Immigration serves as an experimental framework for testing the effects of environmental factors on diseases and on ethnic health disparities.
Good health affects all spheres of life, including labor market performance.
Cons
Immigrants’ initial health advantage deteriorates with time in the host country and converges toward (or below) the health status of native residents.
Disparities between immigrant and native residents may differ across dimensions of health and health metrics and by gender and country of origin and residence.
Immigrants’ self-reports of health conditions may under-report their true health status.
Statistical analyses may be biased downward because they fail to consider sick immigrants who return to their country of origin.
Author's main message
The health status of the host country benefits from immigration, because new immigrants tend to be healthier than native residents and to have healthier habits and lifestyles. Later, as immigrants adjust to the lifestyles and norms of the host country, their health deteriorates. Self-assessed health appears to be an adequate measure for evaluating health status disparities between immigrant and native residents. Because good health affects all spheres of life, including labor market performance, governments should support additional health-care services for immigrants and make health systems more responsive to their needs. The negative effects of immigrant acculturation can be diminished through preventive health practices that can also reduce health-care expenditures.
Motivation
Understanding the determinants of immigrants’ health is important for policymakers and health practitioners today as immigrants are becoming a larger share of the population in many countries. The UN reports that in 2013, some 232 million people lived and worked in a country in which they were not born. Europe hosted 72 million immigrants (31% of the global migrant stock) and the US accommodated 45.8 million (19.7%). Large numbers of immigrants also reside in Saudi Arabia (9.1 million), the United Arab Emirates (7.8 million), Canada (7.3 million), and Australia (5.6 million). Even more impressive is the growth rate in the number of migrants: within the two decades between 1990 and 2013, the total number of migrants rose by more than 77 million, or by 50%. Moreover, immigration will be the driving force in the future growth of the population in many countries. These global demographic trends will play an increasingly central role in shaping health outcomes of the local populations.
It is difficult to isolate the health effects of variations in environments within a country’s native population, but this problem can be overcome by examining immigrants from different countries of origin who now reside in that country. Immigrants offer analytical advantages because they move from one set of environmental conditions (such as development level, lifestyle, religion, behavioral norms, risk factors, climate, and landscape) to a different set. Epidemiology has a tradition of several decades of using migrant patients to isolate environmental effects on diseases [2]. Economists also claim that environmental conditions, in the sending and receiving countries, can explain various aspects of immigrants’ health, both on arrival and later, as well as ethnic disparities in health. However, direct empirical estimates are relatively rare. Adding country-level aggregate measures (relating, for instance, to development level, religion, education, behavioral health risk factors, and health care coverage) to an estimated immigrant health equation could provide insight into various country effects.
The popular perception is that new immigrants can pose a threat to the health of native residents by bringing with them diseases from their country of origin. In the second half of the 19th century, the fear of yellow fever, cholera, and tuberculosis in the US led to the establishment of the first immigrant screening facility (the Marine Hospital Service) on Staten Island in New York. A hundred years later, another dread disease was thought to be related to immigrants: HIV/AIDS [3]. Immigrants are also thought to be a burden on the health system of the host country, which has to fund health services for newly arrived immigrants. These fears are manifested in health screening procedures in several host countries, including Australia, Canada, and the US.
Refined answers to two core questions can provide sound information for decision-making: Are the fears about immigrants’ health status backed by empirical evidence? What role should policy intervention play: is there a need to safeguard native populations or to cater to the special needs of immigrants?
Discussion of pros and cons
Measures of health used in empirical studies
Various health metrics are used to examine health disparities between immigrant and native populations, including mortality rates, life expectancy, disability measures, physical and cognitive functioning limitations, specific health problem/disease diagnosis, body mass index for excess weight and obesity, hospital visits, satisfaction with health, and self-assessed health status. Mortality rates and life expectancy relate to the health status of the community, while the other measures relate to various aspects of an individual’s health.
Following the literature on subjective sense of well-being, self-assessed health status is now commonly used as a metric, based on the finding that individuals are the best evaluators of their own health [1], [4]. Numerous studies have demonstrated that self-assessed health is a good proxy for health status, including among minority populations. Other research reveals that self-assessed health measures accurately reflect physical health problems such as chronic and acute conditions. Self-assessed health status is also highly correlated with death and disease [1]. As a comprehensive overall assessment of an individual’s health condition, self-assessed health status is commonly used as a metric by economists. And it is a good measure to use for native–immigrant comparisons. However, several studies have warned that self-assessed measures may reflect unobserved differences in risk perceptions and in self-reporting biases (residents of different countries may use different response thresholds when placing themselves within ranking scales). Those studies prefer to use more objective measures, such as the body mass index, mortality rates, chronic health conditions, and birth outcomes. Disparities between immigrants and native residents may differ across various dimensions of health, but the evidence based on these objective and less general metrics of health point generally at similar health trajectories [4].
Newly arrived immigrants are healthier than natives
An extensive body of research related to immigrants in a variety of countries (including Australia, Canada, France, Germany, Spain, Sweden, the UK, and the US) has documented that when immigrants arrive in the host country they are healthier than native populations. This phenomenon has been labeled the “healthy immigrant effect.”
Several explanations have been proposed to explain immigrants’ health advantage upon arrival. The theory of positive self-selection of immigrants posits that only the healthiest and most motivated individuals choose to undergo the traumatic experience of migration to a new country; people who are sicker and weaker stay behind [4], [5]. While data shortcomings severely limit the ability to disentangle the role of immigrant selectivity from socio-economic and behavioral factors, some studies have directly tested the self-selection hypothesis by taking advantage of changes in policy, shocks in the country of origin, and within-family analysis to partially isolate immigrant selectivity [6]. Another theory is that medical examinations by immigration authorities in the host countries further screen out less healthy immigrants at the border. Screening started in 1887 in the US [3] and is still the norm in Australia, Canada, and other countries. However, health screening blocks only a small share of immigrants. A third theory is that diets and behaviors are healthier in the home country, including better nutrition and dietary habits, more physical activity, close family and religious ties, and other socially protective factors [7]. Finally, it may be that self-reports of health conditions are under-reported by foreign-born populations, either because they have not yet been diagnosed [4] or because of differences in perceptions about health status.
There is an extensive economic, sociological, and psychological literature on the relationships and positive spillover between good health and various spheres of life, such as labor market performance, subjective well-being, and family relationships. While the positive effects and externalities of immigrants’ good health are valuable and should be reflected in host country policies, they are touched on only lightly in this paper.
Immigrants’ health deterioration with time spent in the host country
Immigrants’ initial health advantage deteriorates with time spent in the host country and converges toward (and even falls below) the health status of native residents. The health decline is especially pronounced against the background of improvements in immigrants’ socio-economic status [1], [4], [5], [7], [8]. Researchers are puzzled by the subsequent health deterioration and have offered several explanations.
Most studies emphasize the role of “negative acculturation”: worsening of dietary styles, adoption of risky behaviors (smoking, alcohol consumption, overeating, lack of physical exercise), and erosion of social and cultural protective factors such as close family and religion ties and social solidarity and stability [4], [7]. Naturally, the acculturation outcomes depend on the gap in behavioral norms between the sending and receiving countries.
Other studies refer to a natural (technical) process of regression toward the mean as immigrants assimilate and converge toward the health status of the local population [4]. This mechanism would suggest that deterioration is inevitable and would leave little room for policy to make a difference.
Another hypothesis is that immigrants tend to use health-care services less frequently than native residents, terminate treatment early, and receive lower-quality health care [7]. Disparities in use of health-care services between immigrants and native residents could stem from differences in health insurance coverage, lack of knowledge about the health-care system, poor knowledge of their rights, and difficulty communicating with health practitioners because of linguistic and cultural barriers. Under-utilization of health-care services, such as preventive health care and screening practices, could have long-term effects on immigrants’ health.
Structural theories based on the historical, political, and economic contexts of immigration suggest that discrimination (stemming from xenophobia, racism, and “otherness”) may be a potential channel leading to a worsening of immigrants’ health over time [9].
The poor conditions under which many immigrants work have been suggested as another significant contributor to the deterioration of immigrants’ health. The hypothesis is that the sorting of immigrants into more dangerous and strenuous occupations can lead to work-related injuries and fatalities and other health problems, and explain the observed deterioration of their health. There is supporting evidence for this labor-market-oriented theory in Germany [8] and the US [10]. The effect of precarious employment is probably magnified by poor living conditions and by the trauma associated with migration.
Another plausible explanation is psychological: middle-aged immigrants and older immigrants who have lived for several decades in the host country may feel severed from their origins and perceive a lower health status than the reality. Missing one’s home country, especially the memories of growing up there and the different geographic settings and climate, can have a negative subconscious effect on perceptions of health status [1].
Immigrants may also change their health reference group over time. When immigrants first arrive, they naturally tend to compare themselves and their health status with that of their compatriots back home. After residing for years in the host country, immigrants can begin to see native residents as their new reference group. If native residents are in better health than immigrants, immigrants may report a lower health status than before, even if their health has not changed [1].
Differences in health by time since migration
Extensive evidence from multiple disciplines and for various countries indicates that immigrants tend to be healthier than native residents when they first arrive, but then their health deteriorates as they spend more time in the host country. Eventually, their health status converges to the level in the local population and even falls below it. Consider the following indicative evidence.
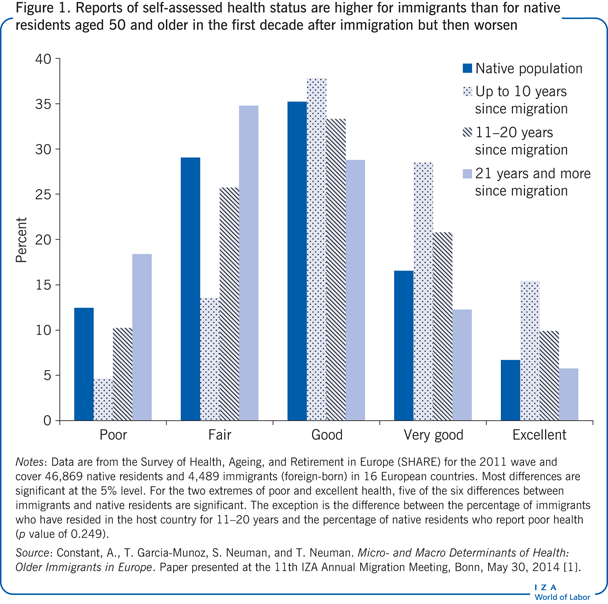
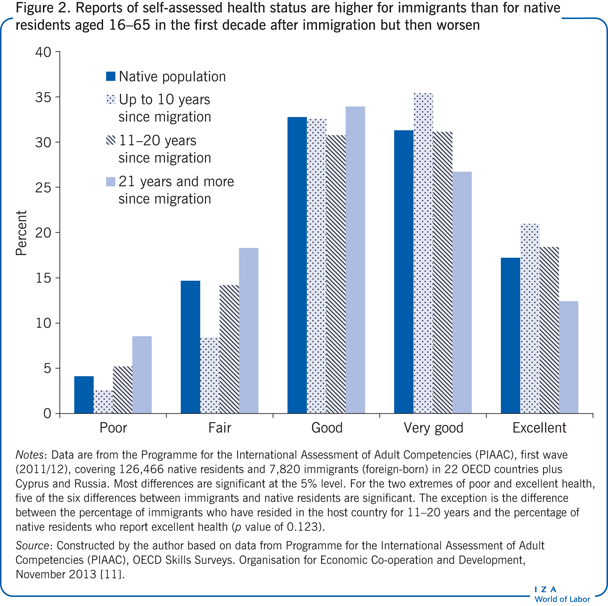
Two recent databases are used to compare the self-assessed health status of immigrants and native residents: the Survey of Health, Ageing, and Retirement in Europe (SHARE), with data on individuals aged 50 and older for 16 European countries [1]; and the Programme for the International Assessment of Adult Competencies (PIAAC), with data on the adult population aged 16–65 in 22 OECD countries, plus Cyprus and Russia (see [11] for data description). The immigrant samples are decomposed by the number of years since migration (up to 10; 11–20; and 21 or more). Immigrants are defined as foreign-born residents.
Although SHARE data are restricted to older individuals, this is the most relevant subgroup for health status analysis and policy implications since health starts to deteriorate around age 50, and this group’s share of the population is growing in virtually all countries.
The distribution of self-assessed health status levels, based on the SHARE data, shows that during the first decade after arrival in the host country, immigrants report higher levels of subjective health than do their native-born counterparts (Figure 1). They report lower relative frequencies for the poor and fair health categories and larger frequencies for the good, very good, and excellent health categories. For instance, only about 5% of new immigrants report a poor health status, compared with about 12% of the native population. At the other end, about 6% of native populations report an excellent health status, compared with about 14% of immigrants who have been in the host country for 10 years or less. As the years since migration increase, reported subjective health decreases, and after more than two decades following migration, it is below the reported levels of the native population.
These are raw health status levels that do not take into account socio-economic disparities between immigrants and native residents (in education, age, marital status, wealth, and other characteristics) that might affect health status. Economists use regression analysis to control for socio-economic disparities and arrive at the net effects of immigration status. Results of such multilevel regression analysis are somewhat different from the raw uncontrolled result. There is still a significant health advantage for immigrants who arrived within the last decade. However, immigrants who have lived in the host country for 11–20 years report a lower health status than native residents, while those who have lived there more than 20 years report a health status that is converging toward that of the native population [1].
For predicting changes in health status over time since migration, the ideal data set would contain longitudinal data; however, the SHARE data set includes only cross-sectional data, which could lead to a mixing of age and cohort effects. However, experimenting with various robustness tests and efforts to disentangle age and cohort effects did not change the basic pattern [1].
To extend and complement the SHARE results, which are restricted to individuals aged 50 and older, analyses were also conducted using the PIAAC data set [11]. The results for raw health status are similar for the extended and more general age spectrum (and a slightly different country mix; Figure 2). Immigrants who arrived less than a decade ago are healthier than the native residents: the percentages of immigrants who report poor and fair health are lower than those of native residents, while the percentages of immigrants who report very good and excellent health are higher (for those who report good health, the percentages are identical). As the time living in the host country lengthens, the reported health status of immigrants deteriorates; after more than two decades, their health status is inferior to that of the local population.
While the focus here is on international migration, it is interesting to note that there is also evidence of the healthy immigrant effect in operation for internal migration (as in south to north, or rural to urban migration in China).
Country-level effects
Immigration provides an experimental framework for testing the effects of country-level determinants of health. Country and environmental effects can be explored by adding country-level aggregate measures for the country of origin and the host country (such as per capita GDP, share of smokers, share of obese individuals, health expenditures as share of GDP, public health-care coverage, educational attainments, major religious denomination, religious intensity, continent) when estimating an immigrant health equation. To test for the possibility that differences in country measures matter (rather than absolute country values) and for asymmetry of positive and negative deviations (of the host country from the country of origin), positive and negative differences can be introduced separately by two different explanatory variables rather than by one variable that relates to the difference between countries.
Estimations for European countries show that reported health is significantly affected by aggregate measures for both the country of origin and the host country (such as per capita GDP, life expectancy, Human Development Index, health expenditures, share of smokers, religiosity), indicating the influence of country-level factors and externalities. For instance, on the positive side, the better infant nutrition, vaccination coverage, and health-care provision in developed countries have long-term positive effects on health during childhood and adolescence, while greater religious intensity, which is believed to lower stress and enhance optimism, also positively affects health status [1], [12]. On the negative side, in countries with a large percentage of smokers, the negative externalities of smoking are more prevalent.
The effects seem to be more pronounced for aggregate measures (such as development level, measured by log of per capita GDP) for the host country. Also, same-size positive and (absolute) negative deviations (per capita GDP of the country of origin minus per capita GDP of the host country) seem to have different impacts on individual self-reported health status (there is asymmetry around the no-difference point). These differential effects can be explained as a variant of the Kahaneman–Tversky loss-aversion theory, with losses suffered because of leaving the country of origin and migrating to a less developed country (a positive deviation) valued more heavily than gains from leaving a less developed country and migrating to a more developed country (a negative deviation) [1].
Limitations and gaps
Trying to generalize the findings on disparities in health status between immigrants and native residents is problematic because observed health differences vary by country of origin and by gender [1]. These differences in aggregate measures for the country of origin can be partially controlled for in regression analyses, while differences in aggregate measures for the host countries can be controlled for in a similar manner using a pooled sample of host countries [1]. Gender can be also introduced as an explanatory variable, including interactions of gender and the core variables.
Another problem concerns potential selection bias, which may arise from the use of cross-sectional data (data at a single point in time) for the statistical analysis. That is because the sample represents only migrants who remained in the host country; migrants who have died or returned to their home country are not represented. Return migrants could include those who become sick and return to their country of origin—known as the “salmon-bias effect.” The salmon-bias effect could explain some unexpected findings, such as the lower mortality rates among foreign-born Mexicans than among the native population in the US [4].
More theoretical guidance is needed to fill the gap between evidence and theory. There are many empirical studies on migration and health outcomes, in particular on the self-selection of healthier migrants and the impact of migration on the health trajectory of migrants. However, the contribution of theoretical models to the understanding of interactions between migration and health is remarkably small. Among the few theoretical models proposed in the literature are a migration model of initial health selectivity and a migration model of subsequent health trajectory (see [4]).
Summary and policy advice
Decades of empirical research do not support the claim that immigrants have negative effects on the health status of the local population. To the contrary, immigrants tend to be healthier than the native population upon arrival and for several years afterwards. Studies find positive externalities resulting from immigrants’ “importation” of healthier behaviors, diets, and lifestyles. Just as important, since health status affects all spheres of life, including labor market performance, immigrants’ better health positively affects their economic adjustment and, consequently, their contribution to the host country economy. Later, as immigrants move into their second decade in the host country, some of these benefits and externalities tend to diminish and even turn negative.
The notion that immigrants are a burden on the health-care system is also not supported by the evidence. New immigrants tend to use fewer health-care services than the native population. A survey conducted in the US in 2003 found that immigrants’ medical expenses were just half those of their US-born counterparts [13]. Even after adjusting for health status, race/ethnicity, gender, health insurance coverage, and other factors, immigrants’ medical expenses averaged about 14–20% less than those of US-born residents. Moreover, immigrants with health insurance had much lower medical expenses than did US-born residents with health insurance, suggesting that—contrary to stereotypes—immigrants’ insurance premiums may be cross-subsidizing the medical expenses of native residents [13].
The low use of health-care services is probably one of the factors behind the deterioration of immigrants’ health the longer they reside in the host country. The disadvantaged access of immigrants to health-care services could be improved by directing more resources to health-care services for immigrants and by making health systems more responsive to their needs. This can be done by reducing linguistic, cultural, and administrative barriers through interpretation and translation services and the use of health mediators; promoting culturally informed models of health care; and training staff in cultural, ethnic, and religious diversity.
The negative effects on the health status of immigrant acculturation can be diminished through preventive health practices such as anti-obesity and anti-smoking campaigns and education programs that promote exercise and healthful diets. Over time, such measures can lower health-care expenditures overall. A 2014 study by the European Centre for International Political Economy estimates that European countries can realize huge savings in health-care expenditures related to obesity by using effective lifestyle weight-management programs to treat obesity today. For example, by 2030, savings in future health-care expenditures related to obesity could be as high as 55% in Sweden, 12% in Spain, 10% in the UK, and 6% in Germany. These preventive programs seem to be more effective for immigrants, who need to re-adjust to the healthier lifestyles they had followed in their countries of origin.
Acknowledgments
The author thanks two anonymous referees and IZA World of Labor editors for many helpful suggestions on earlier drafts. The author also thanks Margard Ody, the IZA Information Manager, for access to many of the publications reviewed for this article. This paper uses data from SHARE wave 4 release 1.1.1, as of March 28th 2013 (DOI: 10.6103/SHARE.w4.111). The SHARE data collection has been primarily funded by the European Commission through the 5th Framework Programme (project QLK6-CT-2001-00360 in the thematic programme Quality of Life), through the 6th Framework Programme (projects SHARE-I3, RII-CT-2006-062193, COMPARE, CIT5- CT-2005-028857, and SHARELIFE, CIT4-CT-2006-028812) and through the 7th Framework Programme (SHARE-PREP, N° 211909, SHARE-LEAP, N° 227822 and SHARE M4, N° 261982). Additional funding from the U.S. National Institute on Aging (U01 AG09740-13S2, P01 AG005842, P01 AG08291, P30 AG12815, R21 AG025169, Y1-AG-4553-01, IAG BSR06-11 and OGHA 04-064) and the German Ministry of Education and Research as well as from various national sources is gratefully acknowledged (see www.share-project.org for a full list of funding institutions).
Competing interests
The IZA World of Labor project is committed to IZA Guiding Principles of Research Integrity. The author declares to have observed these principles.
© Shoshana Neuman