Elevator pitch
Upon arrival in a host country, immigrants often have lower obesity rates (as measured for instance by BMI—body mass index) than their native counterparts do, but these rates converge over time. In light of the worldwide obesity epidemic and the flow of immigrants into host countries with higher obesity rates, it is important to understand the consequences of such assimilation. Policymakers could benefit from a discussion of the impact of immigrant obesity on labor market outcomes and the use of public services. In particular, policies could find ways to improve immigrants’ access to health care for both the prevention and treatment of obesity.
Key findings
Pros
Immigrants arrive with lower BMI and lower obesity rates than those of natives.
Obesity among immigrants remains low in ethnically concentrated areas where acculturation occurs slowly.
Immigrant obesity remains low for males and the college-educated.
In the US there is little evidence of a wage effect of obesity for immigrant men.
Immigrants rarely seek health-care services, so increases in obesity should not result in the overuse of public services.
Cons
Migration generally flows from low- to high-BMI countries. As migrants’ stays increase, they adopt natives’ unhealthy lifestyles and their BMIs approach the higher levels of native populations.
In the UK, lower immigrant obesity rates are associated with higher wages and employment.
In the US, obese immigrant women who stay less than five years incur a wage penalty; In the UK, obese immigrant men experience a significant wage penalty.
The children and grandchildren of immigrants face accelerated obesity rates.
Estimates of “healthy immigrant effects” and the labor market effects of weight may not fully account for factors that can bias the results.
Author's main message
When migrating to countries with high obesity rates, immigrants adopt natives’ behaviors and ultimately face similar obesity risks. Immigrants to the US, for instance, are largely spared labor market penalties for obesity. In the UK, when immigrants’ BMIs remain low they earn more, but this wage advantage is eroded as obesity increases over time. Immigrants seldom seek public-health programs, even in the face of increasing obesity, possibly because they lack access. The challenge for policymakers is to connect immigrants to programs that could reduce obesity and thus ensure more positive labor market outcomes.
Motivation
Obesity is a worldwide epidemic. Rates in many countries have doubled or even tripled since 1980 [1]. Unhealthy weight afflicts 1.9 billion adults and 42 million children under the age of five, who risk serious illness and early death. In addition, overweight and obese individuals may face wage and employment penalties.
Migration from developing to developed countries and from rural to urban areas means migrants often move from areas with lower obesity rates to areas with higher ones. The impact of the obesegenic environment on migrant overweight and obesity rates and outcomes linked to weight status has changed in recent years. Migrants are eating the same unhealthy foods as native populations but do not counterbalance this with physical activity. Unlike their labor market assimilation, immigrants’ adoption of the unhealthy habits of native populations can have negative consequences for them and for their children and grandchildren. The debate over the consquences of migration should thus address changes in obesity rates after migration and their implications for labor market outcomes and public expenditures.
Discussion of pros and cons
The incidence and costs of obesity
The body mass index (BMI) is the typical measurement used to determine a healthy weight. It is calculated as a person’s weight in kilograms divided by the square of his or her height in meters. More than half of all residents of OECD countries are overweight (BMI ≥ 25) and nearly one-fifth are obese (BMI ≥ 30) [2]. Once thought to be a problem only for developed countries, obesity has increased in developing countries at alarming rates. In the US, more than 35% of the adult population was considered obese in 2012. At the same time, obesity rates in Mexico reached an almost equally high 32% [2]. No country has been spared the dramatic increase in obesity of recent decades; not even children have escaped this epidemic. In 2010, over 20% of children between the ages of five and 17 in OECD countries were classified as obese; and these rates have risen over the past decade [2].
Rising obesity is linked to serious health risks. It can lead to increases in diabetes, heart disease, hypertension, and strokes. Nearly 17% of premature deaths are linked to obesity, and the cost of obesity-related health care has been estimated to account for as much as 10% of the overall health expenditures of developed countries. But the impact of rising obesity can reach beyond the obvious health consequences. Accordingly, being overweight or obese can alter important labor market outcomes, such as rates of employment, participation, and wages, and thereby adversely affect some of the more important determinants of economic growth and stability, such as labor supply and productivity.
International patterns of obesity and migration
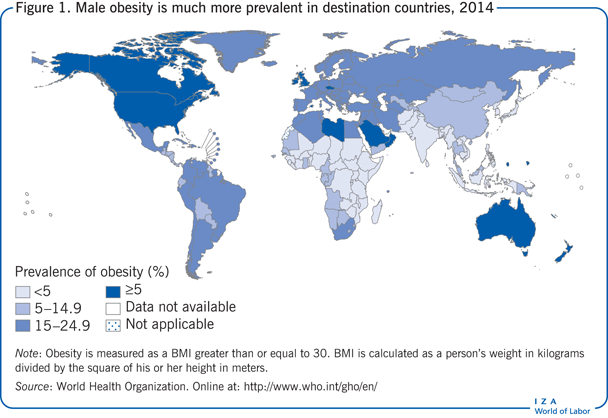
Figure 1 maps out the striking distribution of obesity around the world for 2014. Though these numbers present national obesity rates only for males over the age of 15, women’s obesity and overweight rates are quite similar. The highest obesity rates among males are found in North America, Australia, and in scattered locations in Europe, the Middle East, and North Africa. Although obesity affects less than one-tenth of the population throughout most of Asia and sub-Saharan Africa, these rates continue to increase and threaten to rise above the 10% mark [2].
Many factors influence the decision to migrate, including economic, demographic, and political circumstances of both the (home) country of origin and the destination (host) country, and the attributes of individual migrants. Figure 2 provides migrant counts for the ten destination countries with the largest stocks of migrants and the top ten countries of origin in 2012 [3]. As expected, the US has the largest number of immigrants at more than 45 million. Russia is the second most popular destination, followed by Germany. Both Saudi Arabia and the United Arab Emirates attract male migrants to serve as a substantial portion of their workforce at all skill levels. The next five destination countries, in order, are the UK, France, Canada, Australia, and Spain.
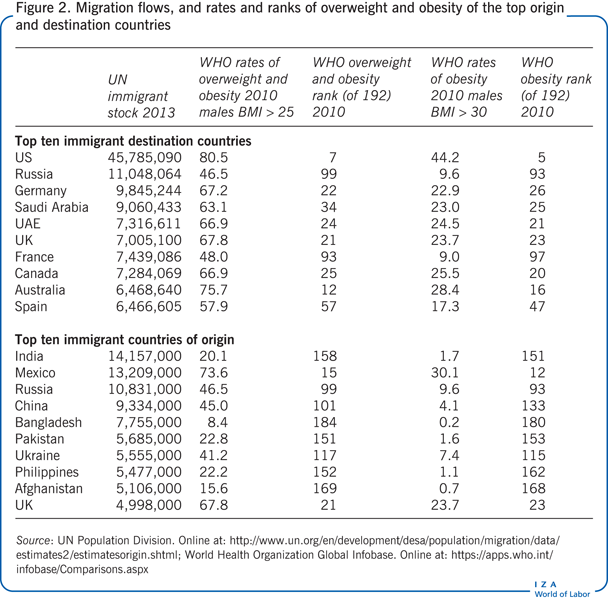
To understand the obesegenic environment immigrants face, column 3 in Figure 2 reports the percentage of the 2010 adult male population whose BMI exceeded the threshold for overweight and obese (BMI > 25) [1]. Column 4 reports the country ranking, based on this rate, out of the 192 countries for which data are available. For example, 80.5% of US males over 15 had a BMI considered to categorize them as overweight or obese, the 7th highest obesity rate among all 192 countries reported. Columns 5 and 6 provide similar reports for the obesity rate (BMI > 30). Each of the ten most attractive host countries had obesity and overweight rates that placed them in the top half of the distribution and, in most cases, their rates were far above the median. Russia and France had the lowest rates among the top ten destination countries, with the 99th and 93rd highest obesity rates respectively among the 192 countries. Most of these destination countries had obesity rates that placed them among the 30 most obese countries in the world and far above most developing countries, such as Afghanistan, Bangladesh, India, and Pakistan.
Where do these immigrants come from? The lower panel of Figure 2 shows the ten countries from which most migrants originate. India supplies the largest number of international migrants, followed by Mexico, Russia, China, Bangladesh, Pakistan, Ukraine, the Philippines, Afghanistan, and the UK. It is noteworthy that Russia and the UK are among the top ten destination and origin countries. In contrast to the overweight and obesity rates of the top destination countries, the top countries of origin for international immigrants are in the lower half of the international obesity distribution, and seven of these are developing countries. For example, in 2010, just over 20% of the adult male Indian population was considered overweight or obese and only 1.7% reached levels considered to be obese. These statistics place India 158th and 151st respectively. All of the popular countries of origin are in the bottom half or middle of the obesity ratings, except for Mexico. Mexicans are the second largest group of international migrants and, in 2010, they had the 15th and 12th highest overweight and obesity rates respectively.
The healthy immigrant effect
The global obesity epidemic and the important role that migration plays in a country’s demographic makeup has prompted a number of studies that examine patterns of overweight and obesity among immigrants upon arrival in the host country and as time since migration increases. These studies use comparisons of BMI between immigrants and natives in immigrants’ host countries as the clinical indicators of overweight and obesity. Although patterns vary somewhat by home and host countries, a number of regular patterns emerge.
Characteristics of immigrants to the US are consistent with the healthy immigrant effect [4], [5], [6], suggesting that recent migrants are healthier than the native-born population. In addition to reporting better initial health behaviors, fewer chronic conditions, and better self-reported health, immigrants are found to have lower BMIs than the native population when they arrive in their host countries and are less likely to be classified as overweight or obese [5], [6]. This relatively low BMI tends to remain low for a time. The health characteristics and transitions of immigrants in Canada and Australia are strikingly similar to those experienced by immigrants in the US [7], [8], particularly when immigrants are living in areas where ethnic groups are concentrated and acculturation is slow.
Patterns of obesity for migrants going to Europe are more mixed; two factors may contribute to this. First, many European countries have a lower incidence of obesity than the US, Canada, and Australia. Second, there are differences in the home country obesity rates of immigrants to Western Europe. Corresponding to the experience of the US, Canada, and Australia, obesity patterns for immigrants in the UK—particularly female immigrants—are consistent with the healthy immigrant effect. It is noteworthy that the UK’s obesity rate is the highest among European countries, so the impact on immigrants in the UK would differ from the impact on immigrants in other European destinations.
The healthy immigrant effect may be rooted in the fact that individuals choosing to migrate face very different circumstances in their home countries compared to those in their new home and have different preferences and behaviors than natives. Recent immigrants will appear healthier if the obesity rates in their home countries are substantially lower, if there is self-selection such that individuals investing in human capital through migration are also healthier, and if migrants are more likely to invest in their own health. It is also possible that immigrant screening processes favor the healthy.
Heterogeneity in the relative fitness of immigrants, based on their country of origin and physiological differences, leads to variations in racial and ethnic patterns of obesity at the time of migration. Although most black, white, Hispanic, and Asian immigrants are healthier and have lower BMIs (and lower rates of obesity) than their native-born counterparts in the US [5], the magnitude of these effects differs across groups. Asian migrants, in particular, display a substantially lower rate of obesity, at the time of migration, than natives, but the relative advantage for Latinos is much smaller because their countries’ obesity rates are larger to begin with [6]. Further, the obesity differential is large for immigrant white and Hispanic men and smaller for immigrant women, especially white and black women [4].
Obesity transition among immigrants
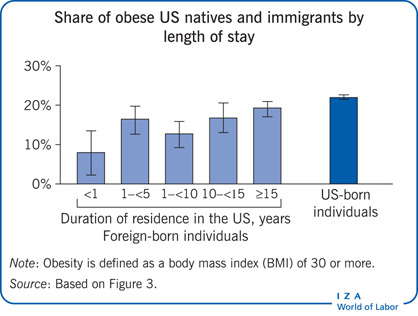
As noted before, migrants to most developed countries are initially healthier and experience lower rates of obesity at the time of migration. But evidence suggests that immigrant health deteriorates and BMI increases as time since migration increases, as illustrated by Figure 3. For many immigrant groups, the healthy weight advantage disappears within ten to 15 years of arrival in a host country [4], [5], but it is difficult to determine whether the rate of increase is related to unhealthy assimilation or whether this would simply have ocurred had the migrants remained in their home country [5].
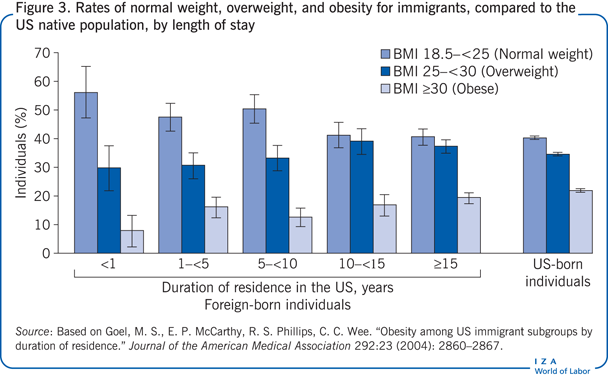
Increases in the obesity rates of immigrants vary across gender and education groups. While obesity rates for immigrant women are closer to those of natives and quickly converge, male immigrants often arrive with substantially lower BMIs and in many cases remain well below the obesity levels of native-born males [3]. Patterns of male immigrant employment may account for this; that is, although physical activity is lower among immigrants, they are more likely to report vigorous physical activity at work. Assimilation patterns also vary by education level. Accordingly, increases in BMI are significantly slower for educated immigrants. College-educated natives also exhibit lower obesity rates, which suggests that education and, likely, the acquistion of knowledge about the health consequences of obesity are protective to both natives and immigrants [9].
There are a number of reasons to expect changes in health as immigrants settle into their new lives. We know they may adopt weight-related behaviors of the native population [6], [9], [10], but this weight gain and associated worsening health could be attributed to either unhealthy food consumption or more sedentary lifestyles. Evidence points to immigrants adopting less-healthy native diets, but they do not exhibit declining physical activity [9], [10]. This means immigrants are acculturating in some ways and not in others, and the manner in which they are acculturating is leading to poor health.
Acculturation and obesity transitions
There is a trade-off between adhering to one’s ethnic identity after migration and assimilating so as to benefit from the resulting improved economic outcomes. Acculturation is the adoption of the language and behaviors of the native population within the host country. It is associated with improved integration into the host labor market and movement into higher-paying jobs. In the area of health, however, acculturation has been found to result in negative outcomes as migrants move from countries where the population is less obese to countries where the population is more obese.
Strong cultural ties and living in areas with high proportions of immigrants have been found to slow the unhealthy assimilation process [6]. In Canada, with an obesity environment similar to that of the US, the larger the ethnic enclave, the slower the transition to native rates of obesity [7]. However, the cost of maintaining one’s ethnic identity and improving one’s health may be slower economic progress.
Immigrants become acculturated to a host country through language acquisition and ethnically integrated social networks; acculturation is also associated with more rapid changes in immigrants’ dietary patterns. In particular, fat consumption and including red meat in one’s diet are more common among those who become more skilled in the native language and integrate natives into their social circles [10]. But, there is less evidence that acculturation is associated with a reduction in physical activity, which would also cause more rapid rates of weight increase. That is, immigrants tend to adopt natives’ diets, but less so their sedentary lifestyles. Nevertheless, health outcomes among immigrant populations are shown to decrease over time [4], [5].
Despite the unhealthy nutrition and weight outcomes related to migrating, immigrants’ use of health-care services is low. Some of this is attributed to a lack of employment-based insurance, for instance, in the US; language barriers also pose difficulties in usage and inhibit the acquisition of health-related information [8]. Although health-care access increases with acculturation, low rates of health-care access by immigrants may result in worsening health with increasing length of stay.
Labor market consequences of obesity for immigrants
Although migration comes with economic benefits, it also comes with costs. So, it is important to understand its impact on immigrants in terms of their health-care consequences and labor-market outcomes, both upon their arrival and as they adopt the behaviors and obesity patterns of natives.
Obese people face many negative consequences in the labor market. If employers or consumers discriminate or if obesity results in lower labor market productivity, then this may result in lower wages or even unemployment. But it is difficult to account for unobservable factors that might contribute to a negative relationship between wages and obesity; for example, lower wages might contribute to obesity because a healthy diet can be more expensive than inexpensive fast food or processed food. This means that rather than obesity leading to lower wages, the reverse could be true. The problem is in isolating the cause and effect.
The evidence is mixed on whether the obese are penalized through lower wages and lack of employment opportunities [11]. In research conducted on non-migrants, US data show that it is primarily obese white women who incur a wage penalty. In Europe, the wage results are less consistent, perhaps due to cultural and labor market differences across countries. Studies for both Europe and the US often report that obese women disproportionately suffer reduced employment [11].
A number of studies have attempted to better estimate whether obesity has a negative impact on wages. These studies used measures of BMI over time and compared the impact of obesity at the individual and sibling level [11]. Even with the use of various statistical techniques, the negative effects of weight on earnings and employment remain but are shown to be smaller after statistical adjustments have been made.
Few researchers have investigated the link between wages and obesity specifically for immigrants; this is perhaps because of the substantial data demands. Nevertheless, two studies analyze the impact of obesity and overweight on wages and employment for recent immigrants to popular destinations. One of these studies examines data on immigrants to the US [12]; while a second study investigates immigrants to the UK [13].
Authors of the US study surveyed the impact of being overweight and obesity on four labor market outcomes: wages, and the probability that an individual is employed, has a white-collar job, or suffers from health-related work limitations [12]. They focus on immigrants from developing countries in Asia and Latin America, countries with obesity rates that are substantially lower than those of native-born Americans. The authors find little evidence of a wage penalty associated with increases in overweight and obesity rates among immigrants who remain in the US. In fact, the only significant association between labor market outcomes and obesity is for immigrant women who have been in the US for a relatively short period of time. Similar to results for native women, obese and overweight women who immigrated in the year prior to the study experienced a reduction in their probability of employment of 18.3 and 9.4 percentage points, respectively. In addition, this study finds a statistically significant association between the BMI of immigrant women living in the US for less than five years and the probability of work limitations.
The study on the UK used a household survey that contained information on immigration status, labor market outcomes, and height and weight [13]. Although immigrants to the UK earned more, on average, than native workers, this differential is accounted for by their higher education levels. Overweight or obese immigrants in the UK receive substantially lower wages [13]. In contrast to penalties for obese natives, this wage penalty is large and significant only for immigrant men. Specifically, obese male immigrants in the UK are paid 20% less than are immigrant men of normal weight. But there is no significant relationship between obesity or being overweight and the probability of employment for immigrants. However, obese male immigrants and overweight and obese female immigrants are more likely to experience work limitations due to disability or ill health. Finally, being overweight or obese reduces the probability of being in a managerial or professional job for native and immigrant men.
The labor market impact of being overweight and obesity differs for immigrants in countries with different institutions and immigration policies and also for different immigrant groups.
Limitations and gaps
The lack of sufficient, accurate, and consistent data poses an impediment to studying obesity and its consequences for immigrants. Such data would include measures of height and weight or body fat, country of origin, timing of migration, and labor market outcomes for a sufficient sample of immigrants, of both genders and all age groups, from a sufficient number of countries. But this is costly and difficult to obtain.
In addition, unmeasurable factors may distort the data. For example, the healthy immigrant effect may be exaggerated because migrants in ill health are likely to return home [7]. Also, patterns of weight status at migration and weight transitions that occur over immigrants’ stays show that BMI may be influenced by the simultaneous impact of age, timing of immigration, and current trends in the weight status of an individual migrant in a group. Studies that carefully account for these factors find that immigrants’ BMIs increase somewhat slower than previously thought, but obesity still increases over time [5], [9].
Finally, to date, most research in this area is limited to some developed countries. Data from other countries would help to give a more comprehensive picture.
Summary and policy advice
Some debates on immigration concern immigrants’ rising overweight and obesity rates, associated illnesses, and the consequent labor-market and health-care costs. But most immigrants arrive with substantially lower BMIs than natives, which points to their better health. Immigrants tend to maintain low BMIs for a substantial period and are less likely to use health-care services, so they do not strain public services. Nevertheless, their obesity rates tend to rise and converge to those of natives as they adopt natives’ habits. This could prove costly to labor-market outcomes and health-care services.
Maintaining one’s ethnic identity and traditional behaviors mitigates against rising BMI. So, dietary acculturation must not progress unimpeded. Policies that provide nutritional interventions can be effective. Policies that maintain ethnic traditions that include foods that are often healthier than those in native diets are often more readily adopted by immigrants. In addition, better information is needed on obesity patterns, earnings potential, and health-care impacts so as to help shape attitudes toward immigration, improve community support, and guide local and national policies. Such policies could include health-promoting information and preventive diagnoses and treatments, a small price to pay to reduce the risks of immigrant obesity and the accompanying productivity losses in the labor market.
Acknowledgments
The author thanks two anonymous referees and the IZA World of Labor editors for many helpful suggestions on earlier drafts.
Competing interests
The IZA World of Labor project is committed to the IZA Guiding Principles of Research Integrity. The author declares to have observed these principles.
© Laura Argys